Tuesday, December 20, 2011
Watch and wait
I did get my blood test results, and while they seem to be showing a flattening out of the liver enzymes, the numbers didn't drop enough to keep me on the trial. So I'm officially off. Where does that leave me? That's not entirely clear. For now, I will keep checking the liver status on a weekly basis. I'll also be getting another MRI in early January to see where things stand. Stay tuned.
Wednesday, December 14, 2011
Liver? Why I hardly....
Humor is always helpful when the news is not ideal. I had another blood test today, and just found out that my liver
numbers are even higher than last week. Not to the point where I need to
be worried about my liver (yet), but it definitely makes it more likely that
I'll get kicked off the trial soon. I'm set up for another blood test on
Monday as per request by Dr. B, though in my mind, if it didn't drop over the
last week, then it's not likely to drop in that short of a time either
(yes, my jaded opinion). He did mention that there have been patients in
other trials who have had the same side effect and unfortunately it took them several
months to drop back down. Of course, I was hoping to be one of those patients whose numbers dropped back to normal in a week or two.
As for other options, the current response from the team is that with a liver issue like this it is not quite a safe time to start Avastin or to have surgery (with anesthesia). The Avastin option was to make this "tumor" disappear, while the surgery was to determine whether it was a tumor after all. I wasn't really looking to do either of those unless there was a growing tumor, so if I do get kicked off this trial, my likely choice might just be to wait until my next MRI and see where we stand (readers' opinions are welcome).
Either way, there will be more discussion after the next blood draw. As he mentioned, it's a day to day process right now, with options and decisions all dependent on the liver numbers.
As for other options, the current response from the team is that with a liver issue like this it is not quite a safe time to start Avastin or to have surgery (with anesthesia). The Avastin option was to make this "tumor" disappear, while the surgery was to determine whether it was a tumor after all. I wasn't really looking to do either of those unless there was a growing tumor, so if I do get kicked off this trial, my likely choice might just be to wait until my next MRI and see where we stand (readers' opinions are welcome).
Either way, there will be more discussion after the next blood draw. As he mentioned, it's a day to day process right now, with options and decisions all dependent on the liver numbers.
Wednesday, December 7, 2011
No change is good change!
Just came back from the latest MRI (which stands for "Most Reasonable Interpretation"). The white spot basically looks the same as the last time. There's still a little more information to gather, but for the most part, I felt good about the results. The next likely step is to get back onto the trial as soon as my liver cooperates. This will hopefully be confirmed tomorrow after Dr. B presents at the Tumor Board and my blood test returns negative. Of course, I'm still in "monitor mode" and will likely have another MRI in 4 weeks or so. However, it is possible that this "thing" will stay dormant for a long time, and I would be perfectly accepting of that as long as it doesn't impose itself!
Overall I guess it was not quite as good as I'd hoped for, but WAY better than I envisioned!
Overall I guess it was not quite as good as I'd hoped for, but WAY better than I envisioned!
Friday, December 2, 2011
Another slight glitch
I just found out that the chemo I'm on has negatively effected my liver, so I've been temporarily "removed". (I swear, mom, it wasn't alcohol!) Next week, when I go in for my MRI, I'll also get some more blood and urine tests and we'll see where things stand. Unfortunately this adds more grey to the situation, since one of the explanations for the potential recurrence was the period of time when I was off chemo due to the swelling...which was going to be "clarified" in my next MRI.
Tuesday, November 22, 2011
Will this be the future?
My friend Grim sent me a link to an interesting talk addressing mutated genes and cancer, in particular brain cancer. Check it out!
A little clarity goes a long way
Yesterday was my appointment with Dr. Berger and Dr. Butowski. Based
on the typical busy schedules, I ended up meeting with both of them
simultaneously. It actually turned out to be very efficient and helpful.
I had already developed a list of questions to alleviate my stress, and
their responses were about as good as I could hope for, given my
current situation. There is still a chance it might not be a tumor, and
the odds could be as good as 50/50 on that front. If it is a
tumor it's still very small, posing little risk to letting it go until
the next MRI in December. If the MRI shows significant growth, then
surgery can still be performed and it is still likely (though not
guaranteed) that I could remain on the current clinical trial. I also
feel less frustrated with "the system" after hearing them explain why it
was not removed during the last surgery. It was not an unfortunate
result of poor communication, but was primarily a more standard approach
from an expert surgeon. Don't cut things out that aren't clearly tumors
and/or clearly safe to attack. If you do, you are opening a world of
hell.
So after all that, I'm heading home to see "The Fam" for Thanksgiving with a much better feeling overall. Happy Turkey Day!
(And thanks again Kate for coming along to help advocate!)
So after all that, I'm heading home to see "The Fam" for Thanksgiving with a much better feeling overall. Happy Turkey Day!
(And thanks again Kate for coming along to help advocate!)
Friday, November 18, 2011
Wednesday, November 16, 2011
Why I might be a little nervous
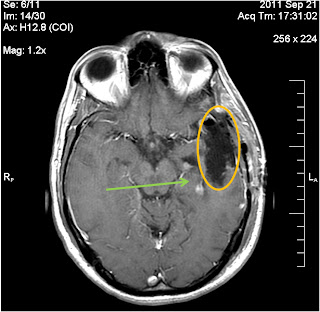
Hear are the images showing what seems to me is another tumor.
Is it a tumor? Sure looks like one in this sequence of images. I'll be meeting with Dr. Berger on Monday, and after that getting another MRI in early December if I'm not already so scared into thinking I need to do something sooner.
 |
| MRI back in early September |
 |
| Post-surgery MRI showing growth in area nearby choroid plexus |
 | |
| Most recent MRI showing further growth (?) of same area. |
Monday, November 14, 2011
Just as I'm starting to climb...
...brain cancer starts to knock me back down.
Today's MRI wasn't the best news. If you recall my worrisome post in early October, there was something discovered post-surgery. That "something" looked slightly larger today, increasing concern that there might be yet another recurrence. Internally it produced a level of frustration I haven't felt since my battle with Kaiser. How could there be a tumor visible in the pre-surgery MRI that wasn't detected soon enough to be removed during surgery? Where was the communication between the surgeons, the oncologists, and the radiation team? Most frustrating is that just as I was starting to get back into the life I love, after playing my first ultimate game, starting to exercise, and seeing the swelling finally disappear permanently; after basically one day of normalcy, it looks like I might be set back to Square 1.
I am still trying to get second opinions from Cedars-Sinai. Unfortunately, at UCSF Dr. Berger is awfully difficult to reach, and the timing couldn't have been worse as everyone seems to be out right now. Hopefully I will get some opinions as to whether this is "something" to continue watching or to extract immediately. Either way, I think it's time to start looking for the next treatment, since the others have all worked so well.
Today's MRI wasn't the best news. If you recall my worrisome post in early October, there was something discovered post-surgery. That "something" looked slightly larger today, increasing concern that there might be yet another recurrence. Internally it produced a level of frustration I haven't felt since my battle with Kaiser. How could there be a tumor visible in the pre-surgery MRI that wasn't detected soon enough to be removed during surgery? Where was the communication between the surgeons, the oncologists, and the radiation team? Most frustrating is that just as I was starting to get back into the life I love, after playing my first ultimate game, starting to exercise, and seeing the swelling finally disappear permanently; after basically one day of normalcy, it looks like I might be set back to Square 1.
I am still trying to get second opinions from Cedars-Sinai. Unfortunately, at UCSF Dr. Berger is awfully difficult to reach, and the timing couldn't have been worse as everyone seems to be out right now. Hopefully I will get some opinions as to whether this is "something" to continue watching or to extract immediately. Either way, I think it's time to start looking for the next treatment, since the others have all worked so well.
Friday, October 28, 2011
Sorry for the delay
I've been so engaged with trying to re-engage, that I wasn't paying much attention to the blog. Basically at this point, things seem to be finally (but slowly) moving in the right direction. The swelling seems to be stable if not shrinking. I haven't had another fever. And I've been forcing myself to exercise to keep myself from going even crazier than y'all expect. In general, if you don't see frequent posts here on the blog, it usually means things are going in the right direction.
Thanks again to all of you who have pulled me through all of this with huge support and kind words!
Thanks again to all of you who have pulled me through all of this with huge support and kind words!
Monday, October 24, 2011
Deja vu?
Or maybe a circular path cycling past the same things over and over?
This morning I met with Dr. Berger, as I did 2 weeks ago exactly. Just like 2 weeks ago, my inflammation was definitely reduced, but not perfect. Just like two weeks ago, I was told by Dr. Berger that it looks great and that I'm allowed to do whatever I want (with the exception of several "details"), but that I should continue to compress the inflammation whenever possible or reasonable. And just like two weeks ago, I left with my head wrapped in an ace bandage.
Unlike two weeks ago, this morning I did not feel sick or wiped out. Let's hope it's not deja vu or an infinite loop, but instead an upward path of a parabola that hit its minimum a couple weekends ago.
This morning I met with Dr. Berger, as I did 2 weeks ago exactly. Just like 2 weeks ago, my inflammation was definitely reduced, but not perfect. Just like two weeks ago, I was told by Dr. Berger that it looks great and that I'm allowed to do whatever I want (with the exception of several "details"), but that I should continue to compress the inflammation whenever possible or reasonable. And just like two weeks ago, I left with my head wrapped in an ace bandage.
Unlike two weeks ago, this morning I did not feel sick or wiped out. Let's hope it's not deja vu or an infinite loop, but instead an upward path of a parabola that hit its minimum a couple weekends ago.
Saturday, October 22, 2011
So I'm not crazy!
Ok, ok, but not for this reason. I was getting worried because it seemed like every evening I was getting close to having a fever again. This time I decided it was time for a little research. After checking it out, I discovered that (a) the range of temperature is relatively broad, and 99.6 or so is actually ok (you also gotta take into account the accuracy of the particular thermometer I have), and (b) your temperature peaks in the evening!
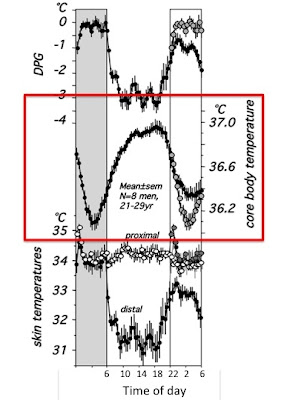
Here's a plot that is a little tough to read, but it does make the point. It's the 2nd plot down with the axis on the right. Phew!
Here's a plot that is a little tough to read, but it does make the point. It's the 2nd plot down with the axis on the right. Phew!
Did it turn out that I was actually right?
First off, with every statement about conditions I make, I expect everyone out there to knock on wood.
I have been home since Thursday evening, and I still haven't shown any fever. The inflammation is definitely not increasing and in fact might be reducing even further. My energy is increasing.
Was my original theory correct? Here is even more potential evidence:
I meet with Dr. Berger on Monday to find out more and also will likely end up back on the chemo, so we'll see how much influence that will have.
I have been home since Thursday evening, and I still haven't shown any fever. The inflammation is definitely not increasing and in fact might be reducing even further. My energy is increasing.
Was my original theory correct? Here is even more potential evidence:
- The fever didn't start until 3 weeks after the surgery. If the surgery got infected, shouldn't it have shown its ugly head a little earlier?
- The inflammation didn't happen until many days after the initial fever. If the inflammation was caused by infection, shouldn't it come before the fever?
- If the inflammation were infected at all, isn't it more likely it would show up within the first 3 days since the assumption was it was caused by the infection?
- Couldn't the inflammation be caused by the either the high temperature fevers I had or by the fact that during that time I was lying down all day every day?
I meet with Dr. Berger on Monday to find out more and also will likely end up back on the chemo, so we'll see how much influence that will have.
Thursday, October 20, 2011
Latest Update
Well today was interesting. This morning (um...yes, first thing) I spoke to a doctor who probably mentioned what was going on, but it wasn't clear what the path was going to be. He said at some point today the whole group would come in to talk with me about it.
Then later in the day BOTH doctors from the Infection Disease group came and saw me, and heard me complain about how little I know and where things might be going. They handled it very well. The next thing they wanted was another MRI to see if there was a sack trapped inside that had some infection which was leading to the fever. I hadn't yet had anyone actually talk with me about when an MRI might be, but I figured if it's not scheduled soon, I'm in for the weekend....
Then there was an earthquake.
Then at some point, one of my great nurses (there were three of them - I can recognize them but can't remember their names) came in to tell me some information: a) They want an MRI sometime "today"; b) I have been taken off the antibiotics; and c) She will find out (and help pressure them) to nail down a time so that if it all looks good I can get out tonight!
Around 5:30 I went in for the MRI, and soon after returning (and eating some sushi with Frodo), I found out the MRI looked great and if I wanted I could leave tonight, or tomorrow. Tonight or tomorrow?!? I want outta here right now! So my wonderful freighbor who's been helping a lot with everything is out here now ready to take me back to my place.
However, their is a slight kink. I have a really good friend who is now an Infective Disease doctor out in Boston, and he's still a little concerned (from my description) that it still might be infected. He named two particular infections that take 5-7 days to form. He actually knows one of the two doctors in the ID dept. here, and so he's gonna "heckle" her to find out what they thought about those. All said, he did agree that going home and keeping an eye on it would be fine. Hopefully they keep watching the culture and that they set it up the right way to test it for these other possible bacteria.
Then later in the day BOTH doctors from the Infection Disease group came and saw me, and heard me complain about how little I know and where things might be going. They handled it very well. The next thing they wanted was another MRI to see if there was a sack trapped inside that had some infection which was leading to the fever. I hadn't yet had anyone actually talk with me about when an MRI might be, but I figured if it's not scheduled soon, I'm in for the weekend....
Then there was an earthquake.
Then at some point, one of my great nurses (there were three of them - I can recognize them but can't remember their names) came in to tell me some information: a) They want an MRI sometime "today"; b) I have been taken off the antibiotics; and c) She will find out (and help pressure them) to nail down a time so that if it all looks good I can get out tonight!
Around 5:30 I went in for the MRI, and soon after returning (and eating some sushi with Frodo), I found out the MRI looked great and if I wanted I could leave tonight, or tomorrow. Tonight or tomorrow?!? I want outta here right now! So my wonderful freighbor who's been helping a lot with everything is out here now ready to take me back to my place.
However, their is a slight kink. I have a really good friend who is now an Infective Disease doctor out in Boston, and he's still a little concerned (from my description) that it still might be infected. He named two particular infections that take 5-7 days to form. He actually knows one of the two doctors in the ID dept. here, and so he's gonna "heckle" her to find out what they thought about those. All said, he did agree that going home and keeping an eye on it would be fine. Hopefully they keep watching the culture and that they set it up the right way to test it for these other possible bacteria.
Wednesday, October 19, 2011
"You are a mystery" - Several UCSF doctors
Here's the latest update. At this point the culture shows no infection. So they are going to check it out one more time tomorrow, and if it still shows nothing they will conclude that it is not infected. However, I've also been told that since I had a fever last night, I cannot have another fever within 24 hours. If I do, I'll be sticking around even longer. So far so good.
As far as the swelling goes, well, unfortunately it's growing again. I was given some potential reasons and lots of ways to approach it. The fluid build up is likely a small hole in the durum that makes it easy for the fluid to leak out from pressure but not get pressed back in. The treatments vary incredibly, and some of them are even a little depressing, so I won't go into that too much at this point, since we still haven't heard specifically from Dr. Berger, who is out of town. I have spoken a lot with Marlene the NP in that department, and she's been great.
All that said, it now seems that the infection theory does not take over. It is still possible that my original theory is correct, with the fever leading to inflammation, although they could also be completely unrelated.
As far as the swelling goes, well, unfortunately it's growing again. I was given some potential reasons and lots of ways to approach it. The fluid build up is likely a small hole in the durum that makes it easy for the fluid to leak out from pressure but not get pressed back in. The treatments vary incredibly, and some of them are even a little depressing, so I won't go into that too much at this point, since we still haven't heard specifically from Dr. Berger, who is out of town. I have spoken a lot with Marlene the NP in that department, and she's been great.
All that said, it now seems that the infection theory does not take over. It is still possible that my original theory is correct, with the fever leading to inflammation, although they could also be completely unrelated.
Tuesday, October 18, 2011
Ooooooooommmmmm...
Well folks, I did get to meet with Dr. Berger yesterday, and he was pretty concerned with the swollen pocket. He drained it all out, sent it off to be cultured, and then sent me into the hospital. I'll be here for at least two days, possibly more. Today I actually spoke to one of the doctors from Berger's team, and he told me that so far they haven't seen any obvious infection from the fluid. I'm a complicated patient apparently. They still stumped as to whether I had an infection at all or what else it might have been. By tomorrow at 3 or so they'll have the final information about the fluid. In the meantime I'm apparently a research project yet again.And no time reserved for shavasana....
Monday, October 17, 2011
Correlation vs. Causality
Am I failing as a "scientist"? I had looked at the correlating evidence, and drew a conclusion that might be entirely wrong. Fever. Achiness. Loss in appetite. Must be flu. Increased pressure in the sack by the surgical area must be due to the high fever. Take Tylenol, reduce fever, feel better. The pressure of the swelling definitely seems to be correlated with the temperature of the fever. Sounds like a good theory.
Until I spoke with Dr. B last night. He's much more concerned with the swelling in the surgical area, and thinks that could be infected, causing the high fevers. When he first mentioned it, it made no sense. Then I let the remainder of my brain think a little bit. Flu? With no coughing? No stuffy nose? And after Tylenol I feel totally fine? Rut roh.
So I'm headed back today to talk to Berger's nurse assistant, and if she tells me he's out and I have to wait until he's around, I'm headed to the ER. A swelling near the brain is not a good thing...even if it is caused by the flu.
Until I spoke with Dr. B last night. He's much more concerned with the swelling in the surgical area, and thinks that could be infected, causing the high fevers. When he first mentioned it, it made no sense. Then I let the remainder of my brain think a little bit. Flu? With no coughing? No stuffy nose? And after Tylenol I feel totally fine? Rut roh.
So I'm headed back today to talk to Berger's nurse assistant, and if she tells me he's out and I have to wait until he's around, I'm headed to the ER. A swelling near the brain is not a good thing...even if it is caused by the flu.
Saturday, October 15, 2011
Yes, I'm over this
Well, I haven't recovered yet, so as you can imagine, I didn't get to make it to the Ride for the Roses to meet Lance. My only saving grace was that I could sit on my couch and watch Michigan beat Michigan State. That didn't work out so well either....
Yesterday I tried to "sweat it out" for awhile. I was carefully monitoring the temperature, and by the time it hit 102, I decided to take the Tylenol. I sacked out early and ended up not taking my chemo (which I'd normally been taking right before bed). I also forgot to put the headband on. I slept a lot better, but not perfectly. When I woke up, I didn't feel wonderful and noticed that my swelling by the surgery had become extremely pressured. First thought was that it might be because I wasn't wearing the headband while laying down to sleep, causing fluid to collect (this I've been told).
I went to take the chemo, and, well, that didn't go so well. As Calvin once said "What goes in, must come out!" So I got in touch with Dr. B and he said I should take a short break to get over this flu. Then I took the Tylenol, and suddenly, after sweating profusely, I started feeling great! As if it were all done! I also noticed that the swollen area by the surgery had loosened up again. After the game, I took a nap, intentionally keeping my headband on and sitting as vertical as possible so the area wouldn't swell again. But after a short time I started to feel chilled. I checked the temperature and it was over 100, and I checked the surgery area and it was swollen again.
So I've been working on a theory. First off, it seems like the fever itself expands the fluid in the surgical area, possibly by generating pressure from the heat? Or perhaps drawing more fluid in there? So I'm still testing that now since I just took Tylenol and am sitting exactly how I was sleeping. Will it get better? Stay tuned! I'm also trying to figure out if taking Tylenol to feel better impairs my immune system from stopping the flu thus extending the total length of cruddiness. I've heard both arguments, but am curious what you all think. I've already tried both!
Yesterday I tried to "sweat it out" for awhile. I was carefully monitoring the temperature, and by the time it hit 102, I decided to take the Tylenol. I sacked out early and ended up not taking my chemo (which I'd normally been taking right before bed). I also forgot to put the headband on. I slept a lot better, but not perfectly. When I woke up, I didn't feel wonderful and noticed that my swelling by the surgery had become extremely pressured. First thought was that it might be because I wasn't wearing the headband while laying down to sleep, causing fluid to collect (this I've been told).
I went to take the chemo, and, well, that didn't go so well. As Calvin once said "What goes in, must come out!" So I got in touch with Dr. B and he said I should take a short break to get over this flu. Then I took the Tylenol, and suddenly, after sweating profusely, I started feeling great! As if it were all done! I also noticed that the swollen area by the surgery had loosened up again. After the game, I took a nap, intentionally keeping my headband on and sitting as vertical as possible so the area wouldn't swell again. But after a short time I started to feel chilled. I checked the temperature and it was over 100, and I checked the surgery area and it was swollen again.
So I've been working on a theory. First off, it seems like the fever itself expands the fluid in the surgical area, possibly by generating pressure from the heat? Or perhaps drawing more fluid in there? So I'm still testing that now since I just took Tylenol and am sitting exactly how I was sleeping. Will it get better? Stay tuned! I'm also trying to figure out if taking Tylenol to feel better impairs my immune system from stopping the flu thus extending the total length of cruddiness. I've heard both arguments, but am curious what you all think. I've already tried both!
Tuesday, October 11, 2011
Timing is everything?!?
Sorry for the delayed update, but I've been recently dealing with some kind of illness. I'm really hoping it's not related to or caused by the chemo, but instead is a simple cold or flu. Not that I'd know, since I haven't been sick in over 5 years and have no idea what to expect (yeah, yeah, I know I'm not counting "cancer" or "drinking too much").
I did meet with Dr. Berger on Monday, and he gave me permission to exercise after checking out the blob of fluid from the surgery. I also asked him about the two "spots" on the MRI, and he had no idea what I was talking about, but was pretty sure if he'd seen something, he would've removed it. I hope I didn't get Dr. B in trouble...though now I'm even more curious - who initially brought it up?
Other than that, I'm just trying to get past whatever this is that keeps rearing its ugly head (insert self-deprecating humor here) so I can still make it to the Ride for the Roses with my buddy Lance! Alas, sometimes timing is everything.
I did meet with Dr. Berger on Monday, and he gave me permission to exercise after checking out the blob of fluid from the surgery. I also asked him about the two "spots" on the MRI, and he had no idea what I was talking about, but was pretty sure if he'd seen something, he would've removed it. I hope I didn't get Dr. B in trouble...though now I'm even more curious - who initially brought it up?
Other than that, I'm just trying to get past whatever this is that keeps rearing its ugly head (insert self-deprecating humor here) so I can still make it to the Ride for the Roses with my buddy Lance! Alas, sometimes timing is everything.
Saturday, October 8, 2011
Thanks "Big Sis"!
Here is an article explaining that choroid plexus changes are not uncommon after surgery on the temporal lobe. Sent to me by my big sister!
Also, I did see 50-50 last night, and it was amazing! An amazing movie with some amazingly supportive friends. Definitely recommended. (And yes, I am willing to see it again).
Also, I did see 50-50 last night, and it was amazing! An amazing movie with some amazingly supportive friends. Definitely recommended. (And yes, I am willing to see it again).
Friday, October 7, 2011
Where things stand
Here are a couple of simplified images from my pre- and post-surgery MRIs. The first picture shows the tumor (red arrow), and also these two white spots that I've been told are likely nothing more than "choroid plexus enhancing in the ventricle" (green arrow). The second picture shows where things were removed and how the white spots are still showing up. They have apparently been there all along, but I think after surgery they expected them not to show up in the contrast image. It could also be a result of radiation. All that said, we need to keep an eye on it, as it could be more tumor (and yes, I will be asking the surgeon why it wasn't taken out in the last surgery). You can also see in the second image the extra "stuff" he took out that wasn't pulling in contrast agent.
Monday, October 3, 2011
Yes, the staples are out
My hope was that once the staples were out, I could start taking steps towards my "normal" life. Unfortunately there was still a lot of swelling, and that's what limits my physical conditioning. Too much heart rate increases the swelling. So I was told officially "you can walk, but no more". For those who know me, you probably know that news like this was not easy to handle.
However there might be a bright side. Almost immediately it seemed like the swelling was dropping. Were the staples the cause of the swelling itself? It makes some sense if you think about where the fluid was (between the skin and the muscles surrounding the skull) and the fact that the staples could have been creating a "pool" to hold the fluid. I'm not quite ready to get excited, but stay tuned....
In other news, I restart the chemo on Wednesday, but in order to do so, I need to once again go through the entire range of baseline testing, including another MRI, an EKG, blood tests, and an eye exam.
At least the weather finally sucks!
However there might be a bright side. Almost immediately it seemed like the swelling was dropping. Were the staples the cause of the swelling itself? It makes some sense if you think about where the fluid was (between the skin and the muscles surrounding the skull) and the fact that the staples could have been creating a "pool" to hold the fluid. I'm not quite ready to get excited, but stay tuned....
In other news, I restart the chemo on Wednesday, but in order to do so, I need to once again go through the entire range of baseline testing, including another MRI, an EKG, blood tests, and an eye exam.
At least the weather finally sucks!
Wednesday, September 28, 2011
50/50 is opening soon!
Here's the link to an interview with Will Reiser on Fresh Air:
http://www.npr.org/2011/09/28/140808566/gordon-levitt-reiser-tackle-50-50-odds
Check it out, and let's go!
http://www.npr.org/2011/09/28/140808566/gordon-levitt-reiser-tackle-50-50-odds
Check it out, and let's go!
Sunday, September 25, 2011
And the winner is...
...T-Bone-Money with her guess of 40 staples! Congratulations! And sorry, there is no prize allowing you to pull them all out of my head. Though it you want to borrow them to torture the Torg, let's talk.
Friday, September 23, 2011
May the words of my mouth and the meditation of my heart...
...not offend too many people. Yes, I've (partially) rejoined the webbed world. Thanks to my mom and sister for filling in and updating (and hopefully still volunteering to step up for reporting when needed?) and my other sister and brother for being there for me from afar. And thanks to my freighbors and friends for all the sweet comments, visits, and contacts during the recovery. It is very much appreciated.
This whole recurrence has definitely reminded me of how awkward it can be to have a brain tumor, at least of the variety that I and some of my fellow "survivors" have. Understandably, many people are surprised by the physical and even mental recovery from a surgery involving what we all think of as the most crucial organ in our bodies. That said, and as much as I love receiving motivating compliments, I guess I don't think that my surgical recovery is that "impressive". Don't take it the wrong way. I'm thrilled at the rate of my recovery, but not completely surprised. In general, the areas of my "brain" being removed are specifically areas no longer in control of my sensory or physical functions. The brain itself isn't a physically sensitive organ, though it can effect sensitivity and physical functioning when damaged in areas controlling other organs or features. Where my personal tumors are hanging out are areas that are fairly non-functional. Well...except when I use them to make excuses....
But to put it simply, I've compared it to a recent procedure my friend "Savory-Em" went through last summer with broken ribs and a punctured lung. If she had been released from the hospital as quickly as I was, and if she were able to perform within days at a similar physical activity level, people should have been shocked. Long-term, however, she should experience close to complete recovery with little to no detriment from the original injury. My experience is the exact opposite in many ways, in that the short term effect of this particular type of cancer, even with surgery, is relatively benign compared to so many other medical issues, whereas the statistical long-term effect is what gives me the greatest concern. Hence the awkwardness of having a brain tumor. It seems like most people's standard expectations don't really match my personal expectations or experience. I should however mention (once again) that I do appreciate all of the wonderful compliments and positive comments I get! This is definitely not a criticism, but more of an explanation of my own perspective.
Many people have been curious about the surgery itself, and since I was actually awake throughout the entire procedure, I figure I should write down my experience now before I forget! The previous surgery at Cedars-Sinai was also an "awake" surgery, but their procedure was very different than this one. Down there I was first put asleep, then awakened for a quick brain mapping, and then put back to sleep for the surgery itself. After the surgery I could not remember anything. Here I was only put to sleep at the very beginning before they began the mapping, and so I basically can remember the rest of the entire process, all the way to the end.
The day before surgery I took a "test" naming simple objects shown to me on a computer screen. The test was essentially meant to determine which images I could very simply name so they could identify which parts of my stimulated cortex were affecting that process. Any image where there was some delay or doubt was removed from the list. I also read through a list of words to test another part of my verbal control.
During the surgery, I was shown these images again and told to name them as quickly as possible, as they were simultaneously stimulating my brain cortex. They also asked me to tell them if I noticed a flash of light towards the edge of my field of view. This did happened a few times and was actually externally stimulated by them in my brain. I never actually felt anything related to the stimulation process itself. The most difficult part of being awake was my general physical condition. Prior to the brain mapping I was under slightly higher sedation. I was still aware of what was happening and could hear conversations and see what was going on, but was free from pain and misery. During the mapping, things got very difficult. I was essentially brought to complete consciousness. My physical position was very uncomfortable, and my throat was very dry making it difficult to speak and breath. The worst was when they noticed that I was "snoring" while breathing. They introduced a pair of tubes into my nostrils to clear my sinuses, and the injection of some nasty fluid led to such an intense shock of pain that I almost jumped off the surgery table (if I hadn't been essentially locked down).
During the mapping process, Dr. Berger tried to comfort me by keeping me up to date on the progress and how close we were to being done. Once the mapping was complete, they were able to sedate me enough to remove the pain and discomfort, though I could still hear everything that was happening. I felt the stitches going in and heard them talking about the process. And then I heard the staples going in, which was unexpected after the stitches! Right up until the end I remained awake, if not alert. I was even awake as they transferred me to the ICU. Though I'm pretty sure soon after that I fell asleep....
So would I do the "awake surgery" again? Difficult question. If I were once again given Dr. Berger's opinion on the effectiveness of this approach for my specific case, no, I would not do it again. It probably did not offer any advantage (as confirmed in his very kind answers to my post-surgery questions), and while it was interesting from a scientific perspective, it was a miserable process to go through. That said, if another "opportunity" presents itself, I will make the decision based on the details of the situation. Or I'll go back to Cedars-Sinai where I couldn't remember a damned thing. Of course, let's hope there aren't any more opportunities showing their ugly faces!
As for the latest update, I had a brief conversation with Dr. B who did confirm that the tumor was real and aggressive, and the extra tumor that Dr. Berger removed was also likely a GBM tumor, sitting there twiddling its thumbs waiting for a chance to spread. Of course they couldn't remove it all, but a lot more is gone now than before! More information to come after an appointment with Dr. B in a week or so and possibly a discussion with Dr. Rudnick down at Cedars-Sinai.
In the meantime, I'll continue to push my recovery back to "normalcy" over the next few weeks. The staples (how many? vote now!) will be removed in about a week. The steroid dosage is already starting to taper and should last another week or so. At some point I will likely be starting the chemo again, with the hope that it does its job with little to no side effects.
Thanks again to everyone who has been there for me live or simply in their thoughts. It's definitely kept me motivated to push forward. My wonderful sister can be relieved of contact now as I do have access to my phone, though if you can't reach me I think she's still ok getting harassed until she heads back to Jersey (I do have AT&T after all, so reaching me was a challenge even before cancer).
Love you all!
"Wolverine" (Hmmm...does that explain the rapid recovery? Stay tuned.)
This whole recurrence has definitely reminded me of how awkward it can be to have a brain tumor, at least of the variety that I and some of my fellow "survivors" have. Understandably, many people are surprised by the physical and even mental recovery from a surgery involving what we all think of as the most crucial organ in our bodies. That said, and as much as I love receiving motivating compliments, I guess I don't think that my surgical recovery is that "impressive". Don't take it the wrong way. I'm thrilled at the rate of my recovery, but not completely surprised. In general, the areas of my "brain" being removed are specifically areas no longer in control of my sensory or physical functions. The brain itself isn't a physically sensitive organ, though it can effect sensitivity and physical functioning when damaged in areas controlling other organs or features. Where my personal tumors are hanging out are areas that are fairly non-functional. Well...except when I use them to make excuses....
But to put it simply, I've compared it to a recent procedure my friend "Savory-Em" went through last summer with broken ribs and a punctured lung. If she had been released from the hospital as quickly as I was, and if she were able to perform within days at a similar physical activity level, people should have been shocked. Long-term, however, she should experience close to complete recovery with little to no detriment from the original injury. My experience is the exact opposite in many ways, in that the short term effect of this particular type of cancer, even with surgery, is relatively benign compared to so many other medical issues, whereas the statistical long-term effect is what gives me the greatest concern. Hence the awkwardness of having a brain tumor. It seems like most people's standard expectations don't really match my personal expectations or experience. I should however mention (once again) that I do appreciate all of the wonderful compliments and positive comments I get! This is definitely not a criticism, but more of an explanation of my own perspective.
Many people have been curious about the surgery itself, and since I was actually awake throughout the entire procedure, I figure I should write down my experience now before I forget! The previous surgery at Cedars-Sinai was also an "awake" surgery, but their procedure was very different than this one. Down there I was first put asleep, then awakened for a quick brain mapping, and then put back to sleep for the surgery itself. After the surgery I could not remember anything. Here I was only put to sleep at the very beginning before they began the mapping, and so I basically can remember the rest of the entire process, all the way to the end.
The day before surgery I took a "test" naming simple objects shown to me on a computer screen. The test was essentially meant to determine which images I could very simply name so they could identify which parts of my stimulated cortex were affecting that process. Any image where there was some delay or doubt was removed from the list. I also read through a list of words to test another part of my verbal control.
During the surgery, I was shown these images again and told to name them as quickly as possible, as they were simultaneously stimulating my brain cortex. They also asked me to tell them if I noticed a flash of light towards the edge of my field of view. This did happened a few times and was actually externally stimulated by them in my brain. I never actually felt anything related to the stimulation process itself. The most difficult part of being awake was my general physical condition. Prior to the brain mapping I was under slightly higher sedation. I was still aware of what was happening and could hear conversations and see what was going on, but was free from pain and misery. During the mapping, things got very difficult. I was essentially brought to complete consciousness. My physical position was very uncomfortable, and my throat was very dry making it difficult to speak and breath. The worst was when they noticed that I was "snoring" while breathing. They introduced a pair of tubes into my nostrils to clear my sinuses, and the injection of some nasty fluid led to such an intense shock of pain that I almost jumped off the surgery table (if I hadn't been essentially locked down).
During the mapping process, Dr. Berger tried to comfort me by keeping me up to date on the progress and how close we were to being done. Once the mapping was complete, they were able to sedate me enough to remove the pain and discomfort, though I could still hear everything that was happening. I felt the stitches going in and heard them talking about the process. And then I heard the staples going in, which was unexpected after the stitches! Right up until the end I remained awake, if not alert. I was even awake as they transferred me to the ICU. Though I'm pretty sure soon after that I fell asleep....
So would I do the "awake surgery" again? Difficult question. If I were once again given Dr. Berger's opinion on the effectiveness of this approach for my specific case, no, I would not do it again. It probably did not offer any advantage (as confirmed in his very kind answers to my post-surgery questions), and while it was interesting from a scientific perspective, it was a miserable process to go through. That said, if another "opportunity" presents itself, I will make the decision based on the details of the situation. Or I'll go back to Cedars-Sinai where I couldn't remember a damned thing. Of course, let's hope there aren't any more opportunities showing their ugly faces!
As for the latest update, I had a brief conversation with Dr. B who did confirm that the tumor was real and aggressive, and the extra tumor that Dr. Berger removed was also likely a GBM tumor, sitting there twiddling its thumbs waiting for a chance to spread. Of course they couldn't remove it all, but a lot more is gone now than before! More information to come after an appointment with Dr. B in a week or so and possibly a discussion with Dr. Rudnick down at Cedars-Sinai.
In the meantime, I'll continue to push my recovery back to "normalcy" over the next few weeks. The staples (how many? vote now!) will be removed in about a week. The steroid dosage is already starting to taper and should last another week or so. At some point I will likely be starting the chemo again, with the hope that it does its job with little to no side effects.
Thanks again to everyone who has been there for me live or simply in their thoughts. It's definitely kept me motivated to push forward. My wonderful sister can be relieved of contact now as I do have access to my phone, though if you can't reach me I think she's still ok getting harassed until she heads back to Jersey (I do have AT&T after all, so reaching me was a challenge even before cancer).
Love you all!
"Wolverine" (Hmmm...does that explain the rapid recovery? Stay tuned.)
Thursday, September 22, 2011
Eric is home!
Yes he got his walking papers today and is back at the manse. He welcomes visitors but please call first as he is also napping a fair amount. And now the moment you have been waiting for--we are opening up the "guess the number of staples" contest again. Enter early and often. But beware--Lil mom keeps trying to cheat and count the staples, so Eric has resorted to wearing a beautiful hat, lovingly knitted for him by his niece....
Wednesday, September 21, 2011
Very latest update
Eric has just been moved from the ICU to his own private room - L 873. He is scheduled for an MRI later today, but right now we don't know what time. Otherwise he's available for visitors. TMI alert: this was his goal for the day.
Tuesday, September 20, 2011
Surgery update
Just a quick update to let you know that everything went well and Eric is already on the mend. He IS sleeping a lot--the combination of getting up at 4 in the morning and 5 hours of brain surgery seems to have depleted his strength a little. He is also still in the ICU but expects to get a regular room tomorrow. And he was happy to hear that Dr. Berger insists that his patients get private rooms! He should be ready to receive visitors tomorrow.
What Eric forgot to tell you.
So the MRI technician wondered if there was anything Eric forgot to tell him that might explain his unusual reactions to the MRI. That's when we remembered the adamantium that permeates his system. Makes sense, right? Right now he's still in surgery. We will update.
Big sis and Lil mom.
Big sis and Lil mom.
Monday, September 19, 2011
It's time
First off, I want to thank everybody who has sent me their best wishes through e-mail, phone messages, or even just thoughts. It really means a lot to me.
Today I went through an MRI, an MS, and an MSI. The MRI once again provided stimulation of my "bird wings". A lot of time was actually spent adjusting the system to reduce the peripheral nerve stimulation, but apparently I'm "unique". I am the only person to date who had the experience I had all the way through the imaging. The conclusion? That system has twice the magnetic power of the other systems I've used (3 Tesla vs. 1.5 Tesla) and apparently I'm quite sensitive....
This was my first exposure to MSI, and it was very interesting. MSI stands for Magnetic Source Imaging, and the idea is simple. You go through a series of sensory and mechanical "test cases" while they monitor the magnetic signals produced by your brain. I was given visual, auditory, and sensory inputs and also had to produce similar outputs. Dr. Berger runs these tests on all of his patients to provide additional mapping to the MRI. It's apparently similar to fMRI (KP - care to comment?) but easier to measure. The room itself looked like a research lab, but the procedure was pretty interesting to me (maybe because it was a research lab?) I'm still hoping to see the match-up between the MRI and the MSI at some point. So someone should remind me, as I have a tendency to forget due to my...never mind.
Of course, I should've remembered what happened down at Cedars-Sinai the day prior to surgery. Yep, once again it was "feduciary day".
Now I've gotta make sure I don't accidentally scratch any of them off tonight.
In other news, I finally met with Dr. Berger and it was really great to talk to him. We are now going to proceed with the "awake surgery". Even though he doesn't seem to think it's necessary, he did say that if I felt more comfortable with that approach, we should go with it. He also mentioned that he was going to take a biopsy of the area where my previous tumor was located, and if he finds something there he will remove it as well. That definitely made us all happy we chose him!
My mom and sister have been watching after me, and will continue to do so over the next several days. I love my family! And I love my friends too! Thanks again for all your support, and I'll catch you on the other side.
Today I went through an MRI, an MS, and an MSI. The MRI once again provided stimulation of my "bird wings". A lot of time was actually spent adjusting the system to reduce the peripheral nerve stimulation, but apparently I'm "unique". I am the only person to date who had the experience I had all the way through the imaging. The conclusion? That system has twice the magnetic power of the other systems I've used (3 Tesla vs. 1.5 Tesla) and apparently I'm quite sensitive....
This was my first exposure to MSI, and it was very interesting. MSI stands for Magnetic Source Imaging, and the idea is simple. You go through a series of sensory and mechanical "test cases" while they monitor the magnetic signals produced by your brain. I was given visual, auditory, and sensory inputs and also had to produce similar outputs. Dr. Berger runs these tests on all of his patients to provide additional mapping to the MRI. It's apparently similar to fMRI (KP - care to comment?) but easier to measure. The room itself looked like a research lab, but the procedure was pretty interesting to me (maybe because it was a research lab?) I'm still hoping to see the match-up between the MRI and the MSI at some point. So someone should remind me, as I have a tendency to forget due to my...never mind.
Of course, I should've remembered what happened down at Cedars-Sinai the day prior to surgery. Yep, once again it was "feduciary day".
Now I've gotta make sure I don't accidentally scratch any of them off tonight.
In other news, I finally met with Dr. Berger and it was really great to talk to him. We are now going to proceed with the "awake surgery". Even though he doesn't seem to think it's necessary, he did say that if I felt more comfortable with that approach, we should go with it. He also mentioned that he was going to take a biopsy of the area where my previous tumor was located, and if he finds something there he will remove it as well. That definitely made us all happy we chose him!
My mom and sister have been watching after me, and will continue to do so over the next several days. I love my family! And I love my friends too! Thanks again for all your support, and I'll catch you on the other side.
Saturday, September 17, 2011
"Prediction is difficult, especially about the future." - Yogi Berra
For those curious, the final plan has been laid out in stone. My "Lil Mom" and "Big Sis" arrive tomorrow morning. Monday I go through the pre-surgery MRI and finally get to meet with Dr. Berger. As many of you know, the two main motivators for battling to get Dr. Berger were his clinical trial and his "awake surgery" technique. I learned yesterday that neither of those will apply to me. The explanations I've heard so far make some sense, but I want to hear it from the surgeons mouth. Until then, I need to shake my disappointment. I've also had many people (rightfully) wonder if I'm getting nervous about the upcoming surgery. I need to report to the hospital by 5 am. Up until now, I never even knew that 5 am existed. So am I nervous? Yes! Mostly about having to get up well before 5 am! In fact, for the surgery itself I'm not sure if I'll even need to be anesthetized....
Beyond that, little is known for sure. I don't know what room I'll be in and I don't know how many days I'll be in the hospital. If I'm lucky and it's anything like the last surgery, I'll be released after only a couple of days. Once things settle in, I'll try to get more specific information up to help promote visitation!
Beyond that, little is known for sure. I don't know what room I'll be in and I don't know how many days I'll be in the hospital. If I'm lucky and it's anything like the last surgery, I'll be released after only a couple of days. Once things settle in, I'll try to get more specific information up to help promote visitation!
Thursday, September 15, 2011
Me? Planning ahead?
Just bought one of these TRX Suspension Training systems! Yeah, yeah, I know. But I was thinking that after surgery I'll be stuck at home wondering how to keep up my energy. Now I can turn to the Ultimate in Bodyweight Training! At least I've got something to dream about in my post-surgical naps.
Tuesday, September 13, 2011
Friday, September 9, 2011
Elvis has left the building
Headed out of the hospital about an hour ago, feeling relatively fine. Haven't noticed any immediate side-effects. I suspect things will accumulate with time, but I'll take it!
And....LIFTOFF!
Just took my first chemo pills. How's that for real-time blogging! Though I suppose I should be tweeting this stuff instead.
I can sense the tumor getting attacked as I type....
I can sense the tumor getting attacked as I type....
Thursday, September 8, 2011
T-minus 17 hours and counting
Tomorrow morning I start the chemo treatment. Unfortunately it sounds like I'll be sitting in the hospital for about 5 hours. Luckily they have wi-fi.
Saturday, September 3, 2011
And the answer is....
From NS: "The B field was high enough to awaken long dormant cells in your head that used to follow earth's magnetic field. The chirp frequency from the MRI was near the right frequency of the chirp from the bird you evolved from so your lats involuntarily flex to flap what used to be your wings."
And my co-worker "Skippy" sent me this. Yes, I'm actually giving "Skippy" credit for something. That *clearly* shows I have a brain tumor....
Now, if I could only fly!
And my co-worker "Skippy" sent me this. Yes, I'm actually giving "Skippy" credit for something. That *clearly* shows I have a brain tumor....
Now, if I could only fly!
Friday, September 2, 2011
Scientists (and science lovers), listen up!
I just had the craziest MRI I've ever had. And I've had a lot of MRIs. Listen to this, and let's figure out what happened!
This MRI was the first one I've had in the main UCSF hospital on the 3rd floor. It was a GE system, which I've been on before. This time, on the second sequence which lasted 7 minutes, I started getting crazy and rapid muscle spasms in my lats! It alternated between the right and left side, and it was happening directly in correlation with the loud chirping noise. Only it stopped in between the high chirps, and it faded away little by little as my position was shifted.
Then, as we got closer to the end of that sequence, it started up again! Slowly increasing until it ended up right where it started. Which made me think that there was some kind of cycling of the position of the brain or the field.
After that, I went through several normal cycles until they started the contrast agent. And with that particular cycle it happened again, only way stronger than the first time! This one actually scared me a little bit. The muscles were rapidly pulsating.
I mentioned it to the tech, and he looked at me like I was crazy. I could only imagine that in this particular MRI there was some (undesirable) electric field in addition to the "normal" magnetic field triggering a particular part of my brain that happens to control the lats. But I'm open to any other theories!
Bring it on....
This MRI was the first one I've had in the main UCSF hospital on the 3rd floor. It was a GE system, which I've been on before. This time, on the second sequence which lasted 7 minutes, I started getting crazy and rapid muscle spasms in my lats! It alternated between the right and left side, and it was happening directly in correlation with the loud chirping noise. Only it stopped in between the high chirps, and it faded away little by little as my position was shifted.
Then, as we got closer to the end of that sequence, it started up again! Slowly increasing until it ended up right where it started. Which made me think that there was some kind of cycling of the position of the brain or the field.
After that, I went through several normal cycles until they started the contrast agent. And with that particular cycle it happened again, only way stronger than the first time! This one actually scared me a little bit. The muscles were rapidly pulsating.
I mentioned it to the tech, and he looked at me like I was crazy. I could only imagine that in this particular MRI there was some (undesirable) electric field in addition to the "normal" magnetic field triggering a particular part of my brain that happens to control the lats. But I'm open to any other theories!
Bring it on....
Wednesday, August 31, 2011
And the winner is?
Exelixis XL785! C'mon down! Your the next contestant on "Kill the Cancer"!
I apologize for the long gap of information since my last post. The thing is, I've had to make seemingly big decisions based on fairly limited information. And as many of you know, I'm not even good at committing to things I know are right! In the end, I stayed true to my general prioritization of the quality of my life, choosing a clinical trial that is unlikely to cause long term toxicity and can be halted at any time if it leads to strong negative impacts.
That said, it is not a placebo. This particular treatment is meant to block the paths in the DNA of cancer cells that tell them: "Time to reproduce!" The plan is to start taking the drug, then have surgery to remove the tumor. The tumor will be looked at to see: (a) is it actually a tumor and (b) did the drug find a way to effect the cells. After recovering from the surgery I'll likely go back on the drug until another tumor pops up, the trial has ended, or I've had enough. I vote for one of the two latter options. All this said, my real hope is that the tumor is just a blip. An evil cell that got left behind on my last surgery and decided to show its ugly face, never to be seen again after the upcoming surgery.
The full schedule has yet to be laid out, but I'm expecting things to accelerate over the next few weeks. I'm hoping to work some optics into the surgery with a trial done by Dr. Berger. (And after that I need to talk to him about "my" original idea for introducing a photocatalyst). Either way, all of this will be local at UCSF, so I'm definitely looking forward to visitors when I head under the knife!
I apologize for the long gap of information since my last post. The thing is, I've had to make seemingly big decisions based on fairly limited information. And as many of you know, I'm not even good at committing to things I know are right! In the end, I stayed true to my general prioritization of the quality of my life, choosing a clinical trial that is unlikely to cause long term toxicity and can be halted at any time if it leads to strong negative impacts.
That said, it is not a placebo. This particular treatment is meant to block the paths in the DNA of cancer cells that tell them: "Time to reproduce!" The plan is to start taking the drug, then have surgery to remove the tumor. The tumor will be looked at to see: (a) is it actually a tumor and (b) did the drug find a way to effect the cells. After recovering from the surgery I'll likely go back on the drug until another tumor pops up, the trial has ended, or I've had enough. I vote for one of the two latter options. All this said, my real hope is that the tumor is just a blip. An evil cell that got left behind on my last surgery and decided to show its ugly face, never to be seen again after the upcoming surgery.
The full schedule has yet to be laid out, but I'm expecting things to accelerate over the next few weeks. I'm hoping to work some optics into the surgery with a trial done by Dr. Berger. (And after that I need to talk to him about "my" original idea for introducing a photocatalyst). Either way, all of this will be local at UCSF, so I'm definitely looking forward to visitors when I head under the knife!
Wednesday, August 24, 2011
(F$#@ Cancer)^3!!!
Yup, it's apparently back. I have to admit, I've been expecting this for about a month. Since the last MRI. In fact, I postponed this MRI until after my kayaking trip with my brother and nephew so I could delay the inevitable. Yup, the summer appears to be over.
So what's next? Well, I'm almost definitely heading back under the knife. I guess the next couple of days will be spent pondering different clinical trials, chemo methods, radiation, etc. Anyone got some other good options? Cause the vaccine didn't seem to fix me.
Does this suck? Yup.
So what's next? Well, I'm almost definitely heading back under the knife. I guess the next couple of days will be spent pondering different clinical trials, chemo methods, radiation, etc. Anyone got some other good options? Cause the vaccine didn't seem to fix me.
Does this suck? Yup.
Tuesday, August 23, 2011
Sunday, July 31, 2011
Thursday, July 28, 2011
Still holding
I spoke with Dr. B today after he presented to the Tumor Board, and as before there isn't much clarity as to what the "white spot" might be. He still thinks it's likely nothing, and even the head of the radiology lab joked that he shouldn't even be allowed to present this tiny spot to the board. But they did all agree that it should be monitored.
An aggressive approach would be to have an MRI in a week or two. To me that seems less useful, since if it's still there and the same, we don't learn anything. Two weeks is not a lot of time to grow. For me, the approach that makes the most sense is to wait a month and then get another MRI. At that point, any changes will become more clear and we'll know what it is and what to do about it. And a month isn't long enough for a tumor to take over my life. Speaking of which, I've got one more month to enjoy. So I'm off!
An aggressive approach would be to have an MRI in a week or two. To me that seems less useful, since if it's still there and the same, we don't learn anything. Two weeks is not a lot of time to grow. For me, the approach that makes the most sense is to wait a month and then get another MRI. At that point, any changes will become more clear and we'll know what it is and what to do about it. And a month isn't long enough for a tumor to take over my life. Speaking of which, I've got one more month to enjoy. So I'm off!
am·big·u·ous /amˈbigyo͞oəs/ - Adjective
1. (of language) Open to more than one interpretation; having a double meaning.
2. Unclear or inexact because a choice between alternatives has not been made.3. My latest MRI
Odds are it's nothing, right? Just a little white spot in an area near the blood vessels. Likely it's just damaged "pipes" leaking the contrast agent. And maybe it wasn't in the previous MRIs because the last three have each been on completely different equipment. Yeah, maybe it was already there and just didn't show up on those other MRIs. Of course, it does look like it could be a growing tumor also....
And that's the conundrum. What to do about white spots that appear in MRIs?
I could try for surgery, but what if it's nothing?
I could try for Avastin, to make it disappear, but then how will I know what it was?
I could try to get a biopsy, but what if they don't pull out the right stuff?
Or I could wait, and watch....
Stay tuned.
Monday, July 25, 2011
Friday, July 8, 2011
A happy anniversary indeed
The "official" two year anniversary of the diagnosis was last night. Though Tuesday felt a little more like the anniversary, since it all went down on the Tuesday after the July 4th weekend. Either way, two years is two years. I've already beaten the stats. Year three, here I come.
Wednesday, June 22, 2011
"Looking good Billy Ray!"
"Feeling good Louis!"
That's about how it is for me right now. In the back of my mind, I understand that this might not last. Statistically it can't last. But statistics are boring, and right now I'm not being forced to take any chemo. In essence I have returned to a physically "normal" life, a life chopped into 6 week segments. And I was just given another reprieve at my MRI today.
I understand people's expectation for cancer to cause physical mutation. Before my "survivorship" began, I generally expected the same. That said, sometimes brain cancer makes for a strange bedfellow - predictively deadly yet often presently invisible. So yes, for now I'm looking good, feeling good, and for the most part, living good.
That's about how it is for me right now. In the back of my mind, I understand that this might not last. Statistically it can't last. But statistics are boring, and right now I'm not being forced to take any chemo. In essence I have returned to a physically "normal" life, a life chopped into 6 week segments. And I was just given another reprieve at my MRI today.
I understand people's expectation for cancer to cause physical mutation. Before my "survivorship" began, I generally expected the same. That said, sometimes brain cancer makes for a strange bedfellow - predictively deadly yet often presently invisible. So yes, for now I'm looking good, feeling good, and for the most part, living good.
Friday, June 3, 2011
A must see movie!
It's about a young person with cancer. For those who are curious about what it's been like, let's go see it!
Thanks Liz Army!
Thanks Liz Army!
Friday, May 27, 2011
Six weeks at a time
I finally got a chance to chat with Dr. B at UCSF after he looked at the MRIs and reports from Cedars-Sinai. It might have been one of the quickest conversations I've ever had with a doc! Basically he said it looked pretty good, though he did mention the same small bright areas that Dr. Rudnick described as well. He then said that I can basically stick with the plan laid out by Cedars-Sinai. Which means...six weeks of freedom! After that, I'll head in for my next MRI, hopeful that I'll get another stellar report which will buy me another round.
Monday, May 16, 2011
The reality of our world....
Today I got news about a couple of people from the brain tumor world. One of them was diagnosed about 6 years ago and was the first person who gave me advice when I was initially diagnosed. He had a recurrence in August. He then entered another trial which led to some surgical complications. From that point on it was a downward spiral that eventually took his life this past weekend.
The other is a friend who had her recurrence diagnosed around the same time as mine. The first clinical trial she was in didn't succeed and she was forced to find another trial and enter repeat surgery only a few months later. She was following in my footsteps in the Cedars-Sinai vaccine trial. This week, on her trip to LA to start the trial, she found out that her tumor had already grown back so fast that she can no longer enter the trial and needs to find a different approach to attack it.
I'm not entirely sure why I'm bringing this up now, besides the obvious fact that I really feel for Jim's friends and family and for Jackie herself and her friends and family. But part of me also sees this as another signal that optimism is important, but so is reality.
The other is a friend who had her recurrence diagnosed around the same time as mine. The first clinical trial she was in didn't succeed and she was forced to find another trial and enter repeat surgery only a few months later. She was following in my footsteps in the Cedars-Sinai vaccine trial. This week, on her trip to LA to start the trial, she found out that her tumor had already grown back so fast that she can no longer enter the trial and needs to find a different approach to attack it.
I'm not entirely sure why I'm bringing this up now, besides the obvious fact that I really feel for Jim's friends and family and for Jackie herself and her friends and family. But part of me also sees this as another signal that optimism is important, but so is reality.
Monday, May 9, 2011
Phew!
It's been about 4 months since my recurrence was diagnosed. It's been about 3 months since it was removed and I began the new clinical trial. It's been about a month since I was motivated to post anything. And it's been about 7 hours since I got the first trial results.
To quote the Cedars-Sinai oncologist, "It think it looks really good" and "You've got the best possible case scenario." Yay!
So what are the next steps? Well, first off I'm going to try to chat with the UCSF docs to see if they can (or even want to) convince me that starting some kind of chemo would be very important. Assuming they can't (or won't), then I'll be checking in again at 6 week intervals during the "crucial time" to see if things are being held at bay.
Phew.
To quote the Cedars-Sinai oncologist, "It think it looks really good" and "You've got the best possible case scenario." Yay!
So what are the next steps? Well, first off I'm going to try to chat with the UCSF docs to see if they can (or even want to) convince me that starting some kind of chemo would be very important. Assuming they can't (or won't), then I'll be checking in again at 6 week intervals during the "crucial time" to see if things are being held at bay.
Phew.
Sunday, April 17, 2011
Why I haven't been updating
"Your pain is the breaking of the shell that encloses your understanding" - Latest fortune cookie
"Sometimes, life sucks" - Anonymous
This has been a particularly challenging year so far. Many of you know the story, but it might be new to others. Right around the day my recurrence was diagnosed, my dad was also diagnosed for adenocarcinoma. We began to battle our cancers in our own ways, though there was some overlap in the treatments. My amazing family switched into high gear, with my two sisters heading out west to take care of me while my brother remained in Michigan to watch over my mom and dad.
Since then our paths were very different. My dad's health generally declined until he just didn't feel like fighting any more. He passed away a week ago Sunday.
My dad was amazing. We all loved him so much, and while nobody lives forever, it still sucks to lose someone so wonderful. And that's why I haven't been updating the blog.
"Sometimes, life sucks" - Anonymous
This has been a particularly challenging year so far. Many of you know the story, but it might be new to others. Right around the day my recurrence was diagnosed, my dad was also diagnosed for adenocarcinoma. We began to battle our cancers in our own ways, though there was some overlap in the treatments. My amazing family switched into high gear, with my two sisters heading out west to take care of me while my brother remained in Michigan to watch over my mom and dad.
Since then our paths were very different. My dad's health generally declined until he just didn't feel like fighting any more. He passed away a week ago Sunday.
My dad was amazing. We all loved him so much, and while nobody lives forever, it still sucks to lose someone so wonderful. And that's why I haven't been updating the blog.
Monday, March 14, 2011
Let the countdown begin!
Today I received the first vaccine shot made from my own home-grown tumor. I have to say, there isn't much excitement to report. In fact, the scariest part was when the flight to LA was showing an hour delay, so I had to wrestle with United to get onto an earlier flight. And the most exciting part was when I finished up at 4:30, and the taxi managed to get me to LAX in under 30 minutes, in spite of commuter traffic!
Beyond that, the event was as follows:
1) Go to lunch at Jerry's Deli and be disappointed that, again, no stars are visiting me
2) Head to the appointment and take Benadryl and Tylenol 30 minutes before taking the vaccine
3) Get the vaccine shot and hold your arm up for 15 minutes
4) Try to sleep in an awkward chair until they wake you up to measure blood pressure and temperature
5) Go home
Of course, as we all know, sometimes no news is good news.
Beyond that, the event was as follows:
1) Go to lunch at Jerry's Deli and be disappointed that, again, no stars are visiting me
2) Head to the appointment and take Benadryl and Tylenol 30 minutes before taking the vaccine
3) Get the vaccine shot and hold your arm up for 15 minutes
4) Try to sleep in an awkward chair until they wake you up to measure blood pressure and temperature
5) Go home
Of course, as we all know, sometimes no news is good news.
Wednesday, March 9, 2011
Interesting Phase 3 Clinical Trial
Here's a video of an interesting treatment explained pretty well. Not for me right now, but maybe down the line....
Sunday, March 6, 2011
2nd verse, same as the first
Last year, on March 6th, I had one of my best days EVER! Well here we are, around the same time, one year later. And I now have evidence to back up the fact that the Huck Cancer tournament is amazing. This year my "bro" headed out from Michigan to join in the fun. Since we each raised over $1,000, and we were on the same team, well...let's just say our taking the championship looked suspiciously like someone fixed the system. In fact, all of the games were pretty close, and he and I were so physically spent by the end, we pretty much hobbled to the party that night and all of the next day (and we'll see about tomorrow too).
Regardless, win or lose, this tournament was incredibly wonderful for me. Once again we had a huge group of amazing volunteers pulling it all together, run primarily by Renata and Coleo, but also with most of the same amazing people as last year. In addition, a lot of my coworkers joined in the fun and helped out tremendously. We also raised over $40,000 for the Livestrong Foundation again. So for all those people who did so much to make this tournament happen (and honestly, I was not a big part of it myself), you deserve tremendous praise and thanks. Therefore, as a representative of the "Cancer Party", I present to you the official statement as follows: Thank you thank you thank you thank you thank you!
Now...time for me to go to bed so my muscles can practice loosening up before I have to walk again.
Regardless, win or lose, this tournament was incredibly wonderful for me. Once again we had a huge group of amazing volunteers pulling it all together, run primarily by Renata and Coleo, but also with most of the same amazing people as last year. In addition, a lot of my coworkers joined in the fun and helped out tremendously. We also raised over $40,000 for the Livestrong Foundation again. So for all those people who did so much to make this tournament happen (and honestly, I was not a big part of it myself), you deserve tremendous praise and thanks. Therefore, as a representative of the "Cancer Party", I present to you the official statement as follows: Thank you thank you thank you thank you thank you!
Now...time for me to go to bed so my muscles can practice loosening up before I have to walk again.
Tuesday, March 1, 2011
Ooops
Sorry. I kinda left people hangin'. So here's a quick summary of answers to questions you probably all have, but thankfully my dear friend Poopapuparama voiced:
1) How many treatments so far?
None. I don't start the actual vaccines until March 14th. They will be day trips to LA taking about 3 hours. I start with some Benadryl and Tylenol, and then I get "the shot". Then they watch my reaction for the rest of the time. I get 3 vaccines total, every other Monday, starting the 14th. Along with the vaccines I need to apply Imiquimod to my (soon to be shaven) armpit for 5 days surrounding the vaccine. This is meant to aggravate my immune system to enhance the vaccines.
None. I don't start the actual vaccines until March 14th. They will be day trips to LA taking about 3 hours. I start with some Benadryl and Tylenol, and then I get "the shot". Then they watch my reaction for the rest of the time. I get 3 vaccines total, every other Monday, starting the 14th. Along with the vaccines I need to apply Imiquimod to my (soon to be shaven) armpit for 5 days surrounding the vaccine. This is meant to aggravate my immune system to enhance the vaccines.
2) How do you feel from them?
We'll see....
We'll see....
3) Is sis still there?
Nope. Big sis left soon after we got back from LA, and "W" left that Saturday. Last week I spent time recuperating, but this week I'm actually back at work! It's going pretty well, though I haven't yet managed to get Jimmy to sing me that song he wrote....
Nope. Big sis left soon after we got back from LA, and "W" left that Saturday. Last week I spent time recuperating, but this week I'm actually back at work! It's going pretty well, though I haven't yet managed to get Jimmy to sing me that song he wrote....
4) How long do the treatments last each time and for how long will you be doing them?
See #1. But there are only 3 treatments, and then after the treatments I have another post-treatment appointment down in LA to see how they might be working and also to discuss the possibility of starting another chemo. Yeah, sure, I'm looking forward to that....
Other than that I'm doing relatively well. A little better every day, but knocking on wood a lot....
See #1. But there are only 3 treatments, and then after the treatments I have another post-treatment appointment down in LA to see how they might be working and also to discuss the possibility of starting another chemo. Yeah, sure, I'm looking forward to that....
Other than that I'm doing relatively well. A little better every day, but knocking on wood a lot....
Wednesday, February 23, 2011
I was SO close!
The plan was to head down to LA for the leukopheresis and removal of the stitches. And the plan itself was executed flawlessly. I headed down there yesterday and met up with H-Lo to be a tourist and grab some dinner in Santa Monica. I spent the night in a hotel that was walking distance to Cedars-Sinai, and woke up early this morning to make it there in time to start the process. The nurse in the blood donation lab was very kind, but also very conservative. I was told under no circumstances was I allowed to move my arms once I was hooked up. This was a little disturbing since my initial thought was that I could sit there for the possible 8 hours reading books, writing e-mails, and watching movies. Luckily the casa Deepistan had given me some movies to bide my time, so I set up my laptop to watch one of my faves, Up. Then I just needed to produce the proper dendritic cells quickly enough so my battery wouldn't just wear out. I managed to finish up in about 3 hours, leaving minutes on my laptop and giving me enough time to rush up to the surgeon's office to get the stitches removed before lunch!
So what am I complaining about? Well...this whole procedure excited me so much because it offered me the chance to finally shower as soon as I got home! And then I get the news - no showering for another 24 hours, AND you should wear a hat to make sure the scar doesn't get infected. Yeah, not much to complain about, I admit...but if you had to hang out with me lately, you might feel the same way.
So what am I complaining about? Well...this whole procedure excited me so much because it offered me the chance to finally shower as soon as I got home! And then I get the news - no showering for another 24 hours, AND you should wear a hat to make sure the scar doesn't get infected. Yeah, not much to complain about, I admit...but if you had to hang out with me lately, you might feel the same way.
Thursday, February 17, 2011
Yep, I'm back!
I arrived back in San Francisco last night, but kept a little on the down low today after having dinner with both sisters and my freighbor. At what most would consider an ungodly hour, my "Big Sis" left this morning and my other sister "W" is sticking around to take care of me until early Saturday morning. I'm a lucky man to have the family I do!
Unfortunately I'm also sometimes a little spacey. Somehow I managed not to record the discussion with the amazing oncologist Dr. Rudnick, whose name, for as much as I like him, must have been carved out with the tumor, as I consistently have not been able to remember it even once since I first met him. And I really do think he's been one of the best oncologists I've talked with so far. (Yes, I did try to use the word "Redneck" to give some association - didn't work so well).
Luckily my "Big Sis" took really good notes that day, so here's a quick summary. Essentially it's believed that the recurrent and obvious tumor sprung from cancer that has been around for a very long time and just recently became more aggressive. The aggressive part of the tumor was growing very rapidly. The number 20% was mentioned for the aggressive, compared with 3% for the non-aggressive part, but to be honest, I can't remember what those referred to at this point. Can you remind me "Big Sis"? Anyway, the part that was really good to hear was that about 99% of the aggressive tumor was removed in the surgery (thanks to the verbal mapping), along with some of the non-aggressive tumor. There is still a very large area of the non-aggressive, spread out tumor, but that's hopefully the part that will be attacked by the vaccine.
In addition, the tumor was tested and showed that it is not sensitive to Temodar. This doesn't necessarily mean I won't go back onto Temodar again, but it does lean in that direction. Apparently on the plus side, "old" tumors like this that aren't really sensitive to Temodar have shown good reactions to the vaccine (we think). And the vaccine might also sensitize the remaining tumor cells to any other types of chemo which have yet to be applied. Of course, if you get a lemon, make lemonade. I try to look at this result and think, well, Temodar made me miserable, so maybe this is a benefit!
My next step is to head down to Lala Land next Tuesday night for a day-long appointment Wednesday. They're going to extract my dendritic cells and replace the rest of my blood. They'll then use those cells and the tumor to make up the vaccine. Also that afternoon I'll get my stitches removed!
About 2 1/2 weeks later I'll head back down there for my first injection of vaccine. This will happen every other week for 3 visits, followed by another MRI and some blood tests checking to see how everything went. Part of this investigation will determine how sensitive my immune system is to the vaccine, giving me some indication to its effectiveness. It will also lead to the decision about whether I'll be picking up another chemo treatment. These conversations will involve Dr. Rudnick and Drs. Clarke and Butowski from UCSF. It's been a pretty positive process so far, and I've really liked the experience I've had down at Cedars-Sinai.
In the meantime, I'm trying to get my life back slowly. I'm still not completely recovered (sheesh, it's been a week, I should be better by now!), but as the steroids reduce, my sleep increases. I do need to slip in some exercise soon just to take advantage of my meds....
Unfortunately I'm also sometimes a little spacey. Somehow I managed not to record the discussion with the amazing oncologist Dr. Rudnick, whose name, for as much as I like him, must have been carved out with the tumor, as I consistently have not been able to remember it even once since I first met him. And I really do think he's been one of the best oncologists I've talked with so far. (Yes, I did try to use the word "Redneck" to give some association - didn't work so well).
Luckily my "Big Sis" took really good notes that day, so here's a quick summary. Essentially it's believed that the recurrent and obvious tumor sprung from cancer that has been around for a very long time and just recently became more aggressive. The aggressive part of the tumor was growing very rapidly. The number 20% was mentioned for the aggressive, compared with 3% for the non-aggressive part, but to be honest, I can't remember what those referred to at this point. Can you remind me "Big Sis"? Anyway, the part that was really good to hear was that about 99% of the aggressive tumor was removed in the surgery (thanks to the verbal mapping), along with some of the non-aggressive tumor. There is still a very large area of the non-aggressive, spread out tumor, but that's hopefully the part that will be attacked by the vaccine.
In addition, the tumor was tested and showed that it is not sensitive to Temodar. This doesn't necessarily mean I won't go back onto Temodar again, but it does lean in that direction. Apparently on the plus side, "old" tumors like this that aren't really sensitive to Temodar have shown good reactions to the vaccine (we think). And the vaccine might also sensitize the remaining tumor cells to any other types of chemo which have yet to be applied. Of course, if you get a lemon, make lemonade. I try to look at this result and think, well, Temodar made me miserable, so maybe this is a benefit!
My next step is to head down to Lala Land next Tuesday night for a day-long appointment Wednesday. They're going to extract my dendritic cells and replace the rest of my blood. They'll then use those cells and the tumor to make up the vaccine. Also that afternoon I'll get my stitches removed!
About 2 1/2 weeks later I'll head back down there for my first injection of vaccine. This will happen every other week for 3 visits, followed by another MRI and some blood tests checking to see how everything went. Part of this investigation will determine how sensitive my immune system is to the vaccine, giving me some indication to its effectiveness. It will also lead to the decision about whether I'll be picking up another chemo treatment. These conversations will involve Dr. Rudnick and Drs. Clarke and Butowski from UCSF. It's been a pretty positive process so far, and I've really liked the experience I've had down at Cedars-Sinai.
In the meantime, I'm trying to get my life back slowly. I'm still not completely recovered (sheesh, it's been a week, I should be better by now!), but as the steroids reduce, my sleep increases. I do need to slip in some exercise soon just to take advantage of my meds....
Tuesday, February 15, 2011
Welcome to the "Hotel California"
You can check out any time you like, but you can never leave....
Our expectation was to head home directly after our meeting this morning, but it turns out the quickest opportunity I have to enter the clinical trial is to start by getting my qualification blood tests tomorrow. Luckily we have such fabulous cousins here willing to let us stick around for another night to start that process! Then in one week I will be heading back down here to have the cells taken out of my immune system for the manufacturing of the vaccine. All of this will be explained in more detail tomorrow, so until then, remember, there's plenty of room at the "Hotel California"....
Our expectation was to head home directly after our meeting this morning, but it turns out the quickest opportunity I have to enter the clinical trial is to start by getting my qualification blood tests tomorrow. Luckily we have such fabulous cousins here willing to let us stick around for another night to start that process! Then in one week I will be heading back down here to have the cells taken out of my immune system for the manufacturing of the vaccine. All of this will be explained in more detail tomorrow, so until then, remember, there's plenty of room at the "Hotel California"....
And the winner is?
The "G. Kravitz Band" (aka "Kravesis") and...my mom! They both guessed ZERO staples, which is how it worked out this time. Stitches only. I guess my original surgeon wasn't lying when he said that the screws and scar would let someone open up easily into the same area of the brain. They didn't even shave a large part of my head, just a strip along the old scar. This definitely relieves my biggest concern, which was whether I could actually change the name of my blog....
Today I'm about to head off for my appointment with Dr. Yu, and then it's back to SF to join the wonderful drizzle. That might be a good thing to keep me inside for more rapid recovery.
Today I'm about to head off for my appointment with Dr. Yu, and then it's back to SF to join the wonderful drizzle. That might be a good thing to keep me inside for more rapid recovery.
Monday, February 14, 2011
Tinseltown!
Today I got to spend a little time seeing the other side of the world, through the frame of a camera in Tinseltown! My cousin here is a music editor working on a film for Warner Brothers, so his he and his wife offered my sister and I a chance to head out there and check out the scene and have some lunch. It was really cool to be able to walk through a far less publicized studio to see what it's like to shoot films there. It's really amazing what it takes to throw together a final piece. We had a really great experience seeing what went behind the scenes and how much fun such a career could be like. We also got to check out the museum, which for several of you out there would've been a dream come true (Peat). The entire top floor was dedicated to the Harry Potter series. Over my head even before the tumors, but very cool nonetheless. I did hit my limit while I was there, but managed to get back "home" in time for a solid nap to recover. In addition to the random energy levels (most likely tied to the steroids I'm on) I'm also noticing a similarity in slight memory loss. Not nearly as bad as the last time, and still awaiting recovery, but frustrating just the same. Weah weah.
Sunday, February 13, 2011
Saturday, February 12, 2011
Yup, time for the update
Yeah, I know, I know. I'm a little late on this post. But I've got a good excuse! It might be old, but it never goes away....
So where have been the last few days? Logan, these are the days of your life!
Tuesday - Feb 8th - Pre-Surgery Day
My "big sister" and I arrived at Cedars-Sinai early for all of my pre-surgery appointments. Initially I met with Dr. Samadi who was in charge of testing me to make sure I was healthy enough to qualify for the surgery. This included an EKG, blood tests, and a chest x-ray. Given our tight schedule I only had time to sneak in the EKG before heading off to an appointment with Dr. Eliashiv to talk about the surgical brain mapping. With her and her cohort I went through a quick test to set a baseline of my "intelligence". She showed me lots of pictures that I was supposed to name, including a compass and a protractor (which I've been mixing up since I was a kid) and an accordion, which for some reason I couldn't remember (even though The Who told me about momma's squeezebox). Other than that I did pretty well. Well enough to use the mapping method as a way to determine which parts of my brain could safely be sliced. The next meeting was with Dr. Yu to talk about the procedure overall and what will happen afterward depending on the results. Dr. Yu and his co-horts were amazing. Seriously, I don't think I've met a surgeon with better "bed-side manner" than Dr. Yu. He's incredibly caring, explicative, kind, and patient. And he also shares a decent sense of humor. My first meeting with him definitely made me feel very comfortable in my decision to head down here to C-S. Well, that and the big Jewish Star on the building. You know how religious I can get. After meeting with Dr. Yu, it was lunchtime and then time to finish up with the rest of the medical tests. The final test (chest x-ray) was in the same location as the MRI that I needed to get, so we managed to pull two tests into one, bumping up the scheduled time for the MRI. This time I had a bunch of stickers adhered to my face (shown below) to spatially map out the MRI image for the surgery. Little did I know, this had to stay on me until I entered surgery. How sexy.... That night I managed to meet up with my dear friend "AE" for dinner and then sack out in preparation for the big day!
Wednesday (and Thursday) - Feb 9th - The "Big" Day
We headed off for C-S early that morning to register for the surgery. I was supposed to be there by around 10:15 for a 2pm surgery. As is typically the case, things took a little longer than expected. However, once I got checked in, I got to meet a few more of the surgeons and also got to meet Dr. "Bob", the anesthesiologist who's worked with Dr. Yu for over a decade. He was incredible. Very communicative, and hilarious. He described all of the positive aspects and the process that the brain mapping procedure went through. Unfortunately he also told me that it was impossible to video record it. There were too many people in too small of a place. There was a slight chance it could be audio recorded, but that depended on others in the room. Basically it was so small that he was practically going to be sitting on my lap. He liked that I was a physicist so he could explain in a little more detail about what was going to be happening. However, the reality of it wasn't quite so exciting for me. As with last time, they injected me with something to sack me out, and then I didn't remember a thing until I was woken up well after. I was told about how witty I was during the brain mapping, with questions such as "What date is Christmas?" to which I answered, "Well...I don't generally celebrate Christmas, since I'm actually Jewish, but if I were to celebrate Christmas, it would be December 25th." Apparently they've had similarly detailed experiences with previous physicists. We're so special (read overly literal?) After surgery I was moved into the ICU for recovery, and remained there for a couple of days. Mainly because the regular rooms were completely full and they couldn't transfer me out! They had a list of rules in the ICU that we followed scrupulously, originally being Midwesterners, but slowly violated as my stay there kept extending unnecessarily. I ended up getting more than one visitor ("big sis" and "AE"), and did "occasionally" eat some sweets for dessert.... While in the ICU, all of my doctors came to visit me at one point or another, including Dr. Yu and Dr. Rudnick who is an oncologist in the department. He, too, was amazing in his description of the procedure, the results, and the upcoming plan.
This is a good time to mention that what I went through was not and will not be a CURE. I'm saying this for myself as much as for everyone else, but realism is key unfortunately. Dr. Rudnick mentioned that for about 30% of the patients the vaccine has a wonderful effect in improving their long term survival, whether it's related to the vaccine on its own or how it improves the effectiveness of future chemo treatments down the line. In addition, so much more of the tumor was removed this time than last, making me very confident that I made the best decision possible. He mentioned that the entirety of the "MRI visible" tumor they removed will be used to make the vaccine, as well as being tested for its response to Temodar. They are also going to test some other cells to see if they represent tumor as well. They are doing a very thorough analysis of what's come out of my brain. More than I've been able to do having owned the brain for over 40 years! Both "big sister" and I agreed that this oncologist was one of the best I've ever dealt with. He explained things very carefully but with good logical background and little vagueness. I'm looking forward to meeting with him again. And while there are some disadvantages to leaving a single company, unified hospital like Kaiser, I couldn't feel better about my decision to be here at Cedars-Sinai with these doctors and nurses. They've all been incredible.
Friday - February 11th - Headed "Home"
I got permission to get released only a couple of days after the surgery, even though I was still being kept in the ICU (due mainly to a crowded hospital). This was basically the same as with the last surgery, except that personally I was doing much better. I was able to walk around with little pain or issues. My memory was much better than last time (yes, I knew how to describe the "tape measures" on my desk at work). And my appetite and understanding of how to handle medications was much better. I was also heading to a much nicer "home"! I cannot praise my cousins here in LA enough. While I'm generally keeping people's personalities as private as I can, my family knows these people well, and they are incredibly special. They have made this entire process completely possible. Even better, they've made it beyond positive. While this was clearly the right decision for this treatment, I cannot even imagine how challenging this would have been to try to pull this off without a wonderful, supportive family taking care of us. Of course, this also marks another time to thank my direct family, especially my "big sister" right now, for all that she's been doing for me day by day. The word "love" is clearly not enough to express how much this means to me.
Saturday - February 12th - Is it the weekend?
So where am I now? Well, I'm still healthy enough to bitch about my status more than I should be. So I guess objectively I'm doing really well, because I hate that I can't (yet) head out to go play ultimate or go bike riding or kayaking. I'm still taking lots of medications, including steroids (enemies beware) that are messing with my sleep quite a bit. I'm not super communicative yet, but working my way back. The current plan is to recover here at my "southern home" up until Tuesday when I have another appointment with the spectacular Dr Yu, and then hopefully will be driving back to my original (and somewhat crowded) home in San Francisco to meet up with my other wonderful sister "W" and my freighbor. For those of you living there, visits will of course be welcome! Though the timing and extension of them might be limited depending on how I'm doing (I am optimistic however!)
In other news, my family is still dealing with one heck of a month. My dad had a brain radiation surgery for a metatastic cancer he had a day after my surgery. His brain surgery went well, but soon after he was suffering from a challenging bowel issue leading to digestive issues. The latest news on that is that it's under control, but of course we are still concerned with his conditions all initially created by the stupid cancer. So, I'll remind you all that cancer really does suck! And there's still going to be an ultimate frisbee tournament developed to raise money to fight all kinds of cancer. A description of the tournament can be found at http://www.huckcancer.org. I am still hoping to be recovered well enough to play in it, and am also raising money for the cause, which is the Lance Armstrong Foundation (a really amazing group). Feel free to donate here!
So where have been the last few days? Logan, these are the days of your life!
Tuesday - Feb 8th - Pre-Surgery Day
My "big sister" and I arrived at Cedars-Sinai early for all of my pre-surgery appointments. Initially I met with Dr. Samadi who was in charge of testing me to make sure I was healthy enough to qualify for the surgery. This included an EKG, blood tests, and a chest x-ray. Given our tight schedule I only had time to sneak in the EKG before heading off to an appointment with Dr. Eliashiv to talk about the surgical brain mapping. With her and her cohort I went through a quick test to set a baseline of my "intelligence". She showed me lots of pictures that I was supposed to name, including a compass and a protractor (which I've been mixing up since I was a kid) and an accordion, which for some reason I couldn't remember (even though The Who told me about momma's squeezebox). Other than that I did pretty well. Well enough to use the mapping method as a way to determine which parts of my brain could safely be sliced. The next meeting was with Dr. Yu to talk about the procedure overall and what will happen afterward depending on the results. Dr. Yu and his co-horts were amazing. Seriously, I don't think I've met a surgeon with better "bed-side manner" than Dr. Yu. He's incredibly caring, explicative, kind, and patient. And he also shares a decent sense of humor. My first meeting with him definitely made me feel very comfortable in my decision to head down here to C-S. Well, that and the big Jewish Star on the building. You know how religious I can get. After meeting with Dr. Yu, it was lunchtime and then time to finish up with the rest of the medical tests. The final test (chest x-ray) was in the same location as the MRI that I needed to get, so we managed to pull two tests into one, bumping up the scheduled time for the MRI. This time I had a bunch of stickers adhered to my face (shown below) to spatially map out the MRI image for the surgery. Little did I know, this had to stay on me until I entered surgery. How sexy.... That night I managed to meet up with my dear friend "AE" for dinner and then sack out in preparation for the big day!
Wednesday (and Thursday) - Feb 9th - The "Big" Day
We headed off for C-S early that morning to register for the surgery. I was supposed to be there by around 10:15 for a 2pm surgery. As is typically the case, things took a little longer than expected. However, once I got checked in, I got to meet a few more of the surgeons and also got to meet Dr. "Bob", the anesthesiologist who's worked with Dr. Yu for over a decade. He was incredible. Very communicative, and hilarious. He described all of the positive aspects and the process that the brain mapping procedure went through. Unfortunately he also told me that it was impossible to video record it. There were too many people in too small of a place. There was a slight chance it could be audio recorded, but that depended on others in the room. Basically it was so small that he was practically going to be sitting on my lap. He liked that I was a physicist so he could explain in a little more detail about what was going to be happening. However, the reality of it wasn't quite so exciting for me. As with last time, they injected me with something to sack me out, and then I didn't remember a thing until I was woken up well after. I was told about how witty I was during the brain mapping, with questions such as "What date is Christmas?" to which I answered, "Well...I don't generally celebrate Christmas, since I'm actually Jewish, but if I were to celebrate Christmas, it would be December 25th." Apparently they've had similarly detailed experiences with previous physicists. We're so special (read overly literal?) After surgery I was moved into the ICU for recovery, and remained there for a couple of days. Mainly because the regular rooms were completely full and they couldn't transfer me out! They had a list of rules in the ICU that we followed scrupulously, originally being Midwesterners, but slowly violated as my stay there kept extending unnecessarily. I ended up getting more than one visitor ("big sis" and "AE"), and did "occasionally" eat some sweets for dessert.... While in the ICU, all of my doctors came to visit me at one point or another, including Dr. Yu and Dr. Rudnick who is an oncologist in the department. He, too, was amazing in his description of the procedure, the results, and the upcoming plan.
This is a good time to mention that what I went through was not and will not be a CURE. I'm saying this for myself as much as for everyone else, but realism is key unfortunately. Dr. Rudnick mentioned that for about 30% of the patients the vaccine has a wonderful effect in improving their long term survival, whether it's related to the vaccine on its own or how it improves the effectiveness of future chemo treatments down the line. In addition, so much more of the tumor was removed this time than last, making me very confident that I made the best decision possible. He mentioned that the entirety of the "MRI visible" tumor they removed will be used to make the vaccine, as well as being tested for its response to Temodar. They are also going to test some other cells to see if they represent tumor as well. They are doing a very thorough analysis of what's come out of my brain. More than I've been able to do having owned the brain for over 40 years! Both "big sister" and I agreed that this oncologist was one of the best I've ever dealt with. He explained things very carefully but with good logical background and little vagueness. I'm looking forward to meeting with him again. And while there are some disadvantages to leaving a single company, unified hospital like Kaiser, I couldn't feel better about my decision to be here at Cedars-Sinai with these doctors and nurses. They've all been incredible.
Friday - February 11th - Headed "Home"
I got permission to get released only a couple of days after the surgery, even though I was still being kept in the ICU (due mainly to a crowded hospital). This was basically the same as with the last surgery, except that personally I was doing much better. I was able to walk around with little pain or issues. My memory was much better than last time (yes, I knew how to describe the "tape measures" on my desk at work). And my appetite and understanding of how to handle medications was much better. I was also heading to a much nicer "home"! I cannot praise my cousins here in LA enough. While I'm generally keeping people's personalities as private as I can, my family knows these people well, and they are incredibly special. They have made this entire process completely possible. Even better, they've made it beyond positive. While this was clearly the right decision for this treatment, I cannot even imagine how challenging this would have been to try to pull this off without a wonderful, supportive family taking care of us. Of course, this also marks another time to thank my direct family, especially my "big sister" right now, for all that she's been doing for me day by day. The word "love" is clearly not enough to express how much this means to me.
Saturday - February 12th - Is it the weekend?
So where am I now? Well, I'm still healthy enough to bitch about my status more than I should be. So I guess objectively I'm doing really well, because I hate that I can't (yet) head out to go play ultimate or go bike riding or kayaking. I'm still taking lots of medications, including steroids (enemies beware) that are messing with my sleep quite a bit. I'm not super communicative yet, but working my way back. The current plan is to recover here at my "southern home" up until Tuesday when I have another appointment with the spectacular Dr Yu, and then hopefully will be driving back to my original (and somewhat crowded) home in San Francisco to meet up with my other wonderful sister "W" and my freighbor. For those of you living there, visits will of course be welcome! Though the timing and extension of them might be limited depending on how I'm doing (I am optimistic however!)
In other news, my family is still dealing with one heck of a month. My dad had a brain radiation surgery for a metatastic cancer he had a day after my surgery. His brain surgery went well, but soon after he was suffering from a challenging bowel issue leading to digestive issues. The latest news on that is that it's under control, but of course we are still concerned with his conditions all initially created by the stupid cancer. So, I'll remind you all that cancer really does suck! And there's still going to be an ultimate frisbee tournament developed to raise money to fight all kinds of cancer. A description of the tournament can be found at http://www.huckcancer.org. I am still hoping to be recovered well enough to play in it, and am also raising money for the cause, which is the Lance Armstrong Foundation (a really amazing group). Feel free to donate here!
Friday, February 11, 2011
Thursday, February 10, 2011
Another update from Big Sis
I spent the day with Eric--he is totally amazing! He looks great, is walking around, eating normally, flirting with the nurses....and conniving to get an early discharge. We think that may happen tomorrow. Unfortunately, because the hospital is SO popular, Eric had to stay in ICU even though he doesn't need intensive care. However, he followed the ICU rules of no cell phones or computers which is why he has been incommunicado. Hopefully tomorrow he will be reunited with his gadgets and I can turn this blog back over to him.
On the medical front, Dr. Yu says that the post-op MRI looked really great, so that is very good news. He also regaled us with stories of the embarrassing things Eric said when they woke him up during surgery to probe his brain. And what were they? Well, you'll have to ask Eric--all I can say is that apparently physicists are quite erudite even under anesthesia.
Still no celebrity visits, but one nurse told Eric that as far as she was concerned, he was a star. So clearly the surgery didn't affect his charm factor.
On the medical front, Dr. Yu says that the post-op MRI looked really great, so that is very good news. He also regaled us with stories of the embarrassing things Eric said when they woke him up during surgery to probe his brain. And what were they? Well, you'll have to ask Eric--all I can say is that apparently physicists are quite erudite even under anesthesia.
Still no celebrity visits, but one nurse told Eric that as far as she was concerned, he was a star. So clearly the surgery didn't affect his charm factor.
Wednesday, February 9, 2011
Update from Big Sis
I just got word from Eric's doctor that he did great during the surgery. They were able to wake him up in the middle and perform a test that involved showing him cards with pictures while they stimulated areas of the brain. Not surprisingly, Eric passed the test with flying colors, enabling the doctor to target tumor areas rather than important brain areas. Doctor Yu believes he got pretty much all of the tumor out (he thinks it IS tumor and not necrotic cells) and that there will be plenty for the vaccine. Eric was in great spirits before the surgery, endearing himself to the medical staff with his scientific curiosity about the technical aspects of the procedure (and the chocolate he spread around didn't hurt either!)
Eric will likely be in the ICU tonight, which means that he had to be surgically separated from his cell phone and his computer. Therefore, please don't be offended when he doesn't respond to texts, e-mails or calls. I will be able to return his electronics to him most likely tomorrow.
On another note, there was a celebrity sighting today in the waiting area while Eric was under the knife--an actress from Designing Women. I was not able to tackle her and get her to visit Eric, but I will try to be better prepared from now on.
Eric will likely be in the ICU tonight, which means that he had to be surgically separated from his cell phone and his computer. Therefore, please don't be offended when he doesn't respond to texts, e-mails or calls. I will be able to return his electronics to him most likely tomorrow.
On another note, there was a celebrity sighting today in the waiting area while Eric was under the knife--an actress from Designing Women. I was not able to tackle her and get her to visit Eric, but I will try to be better prepared from now on.
Tuesday, February 8, 2011
Puttin' on the Ritz
Today has been one crazy day. My "Big Sis" and I had to cruise around Cedars-Sinai for the first time to put to rest all of the appointments and tests required to enter surgery tomorrow. We started with the pre-op appointment to test my blood, urine, lungs, and heart to make sure I'm healthy enough for a major surgery. In the middle of taking those tests,
I had an appointment to learn more about my "awake" time during the surgery. This is very cool. After they open my head, they'll wake me up and start probing my brain. While they're probing they'll show me pictures and ask me questions to determine which parts of the brain they can carve out, and which parts they need to leave behind. I really want them to videotape this, but I don't think that'll happen. I also got to finally meet Dr. Yu, and this increased my confidence even more. Not only does he clearly know his stuff, but he also has amazing bedside manner! In fact, the entire hospital so far has been incredible. Whenever we looked lost, someone would stop and ask us if we needed help. That said, I still haven't run into a Hollywood star.
The last item on my list today was a pre-op MRI. For the first time in my history, they marked locations on my head that will better guide the surgery. These plugs they stuck to me make me look like...well...you guessed it.
 FRANKENERIC!!!!!
FRANKENERIC!!!!!
These need to stay on until the surgery tomorrow, which starts around noon and should end around 4. That means no shower tomorrow.
Not sure when I'll be ready to update the blog, but I'll try. Or maybe I'll beg a family member to post my status....
ps - Thank you all SO much for all the great messages I've received via e-mail, texting, voicemail, etc. Sorry I haven't gotten back to you directly yet, but it's meant a lot to me!
pps - Let's hope they don't accidentally replace my brain with Abby's....
I had an appointment to learn more about my "awake" time during the surgery. This is very cool. After they open my head, they'll wake me up and start probing my brain. While they're probing they'll show me pictures and ask me questions to determine which parts of the brain they can carve out, and which parts they need to leave behind. I really want them to videotape this, but I don't think that'll happen. I also got to finally meet Dr. Yu, and this increased my confidence even more. Not only does he clearly know his stuff, but he also has amazing bedside manner! In fact, the entire hospital so far has been incredible. Whenever we looked lost, someone would stop and ask us if we needed help. That said, I still haven't run into a Hollywood star.
The last item on my list today was a pre-op MRI. For the first time in my history, they marked locations on my head that will better guide the surgery. These plugs they stuck to me make me look like...well...you guessed it.
 FRANKENERIC!!!!!
FRANKENERIC!!!!!These need to stay on until the surgery tomorrow, which starts around noon and should end around 4. That means no shower tomorrow.
Not sure when I'll be ready to update the blog, but I'll try. Or maybe I'll beg a family member to post my status....
ps - Thank you all SO much for all the great messages I've received via e-mail, texting, voicemail, etc. Sorry I haven't gotten back to you directly yet, but it's meant a lot to me!
pps - Let's hope they don't accidentally replace my brain with Abby's....
Monday, February 7, 2011
Sunday, February 6, 2011
Heading to LA-LA Land!
My sister Donna just got in today from the snowy and blustery East Coast, and tomorrow we head south to LA to get this project moving! I'll try to keep things up to date as they change, and so far, they haven't.
Sunday, January 30, 2011
Wanna meet my next surgeon?
Here's a great video with Dr. Yu talking about vaccine trials:
http://www.virtualtrials.com/VIDEO2010.cfm?video=1
http://www.virtualtrials.com/VIDEO2010.cfm?video=1
Thursday, January 27, 2011
Lets Get 'Er Done!
In spite of my typical inability to plan ahead, I've finally got...well...a plan! I will be heading down to Cedars-Sinai in Los Angeles on February 7th with (at least) one of my sisters. On the 8th I'll have a meeting with Dr. Yu to discuss my treatment, and then on the 9th I'll have the craniotomy to remove the tumor. Once I recover enough, I'll head back up to SF to recuperate with (at least) one of my sisters. Meanwhile, assuming the tumor is large enough, it will be mashed around with some of my dendritic cells to create a vaccine which I will get poked with about 3-4 weeks after. How's THAT for a plan!
As for the rest of my stressful time, let's just say that in spite of the brilliant and logical arguments presented by me and my sisters, Kaiser held their ground as expected. That said, I've managed to work around them and all is well and good in coverage-land.
While I was struggling through the decision making process, I did contact Livestrong, the organization for which Huck Cancer was (and is) raising money. They were incredibly empathetic and extremely helpful! So with that, I hereby announce a different "recurrence". If the tumors are going to repeat themselves, then so is the battle to fight them!
I give you: Huck Cancer II - Yes, We Still Give A Huck !!!
Spread the word, share the hate. And please donate.
As for the rest of my stressful time, let's just say that in spite of the brilliant and logical arguments presented by me and my sisters, Kaiser held their ground as expected. That said, I've managed to work around them and all is well and good in coverage-land.
While I was struggling through the decision making process, I did contact Livestrong, the organization for which Huck Cancer was (and is) raising money. They were incredibly empathetic and extremely helpful! So with that, I hereby announce a different "recurrence". If the tumors are going to repeat themselves, then so is the battle to fight them!
I give you: Huck Cancer II - Yes, We Still Give A Huck !!!
Spread the word, share the hate. And please donate.
Monday, January 24, 2011
I finally understand...
...why some people enjoy watching soap operas. It's a way to let your thoughts drift away from the craziness in your own life into the fantasy mayhem exposed in every episode. Add humor to the mix, and it just might absorb every free minute that "someone" has available. It also might explain why "someone" hasn't been keeping the blog as current as people might like. Just remember, "These are the Tates, and these are the Campbells, and this is...."
Thursday, January 20, 2011
Scrambled brain, scrambled days
Sorry for the delay in updating y'all. The last few days have been a whirlwind, and I'm not even sure where to start. From the clinical trial side of things, I have now finally spoken with Dr. Parsa at UCSF, and for his oncophage trial it sounds like I have a >50% chance of having enough tumor to produce vaccine. Yes, almost a coin flip. He also mentioned that if I were to go on the Toca-511 trial, I would likely eliminate any chances I might have in the future for a vaccine trial. This was the last nail in the Tocagen coffin. I am planning on speaking with Dr. Liau from UCLA tomorrow to find out a little bit more about their two vaccine trials, and soon after that I hope to make a decision. After all of this, I think I am still leaning towards the Cedars-Sinai trial, assuming that it does seem as effective as the UCLA trial. I'm likely not willing to take the "coin-flip" risk with the UCSF trial.
The rest of my time has primarily been spent trying to figure out how to pay for the trial. My "insurance" company, Kaiser Permanente, will not pay for the out-of-network surgery required by all of these trials. They would be happy to allow me into the trial if they could perform the surgery themselves. However, none of the trials can allow that due to FDA regulation. So here I sit in the middle of what clearly seems to me to be a financial clampdown of Kaiser. I submitted an appeal to their denial, and my appeal was...well...denied. I was offered, however, a personal 10 minute response to the deny-ers, live and in person. Today.
Now, according to them, I was denied coverage of this trial because "referral to the clinical trials [I] have requested is not medically indicated at this time because they lack efficacy in peer reviewed literature." And furthermore, "[My] treating neuro-oncologist...has offered to [me] treatment with a clinical trial with Tocagen or treatment with avastin/CCNU, which [I] have declined."
So, in 10 minutes I need to prove that (a) the trials I'm considering have strong evidence of efficacy (including peer reviewed literature), (b) the trials that are acceptable to Kaiser show far less efficacy than the vaccine trials, but require little financial contribution by Kaiser, thus indicating that their decisions are financial, not medical, and (c) the main thing that Kaiser is denying, the surgery required by the clinical trial, is, in and of itself, the most medically indicated treatment I could have given my current condition. Yes, that's a lot. My first step? Send out an e-mail to my family that says, "I need help!" Immediately they kicked into high gear, finding me several great peer reviewed articles and other information. I also touched base with the "Sue"-club, two friends who have a lot of experience dealing with Kaiser and with funding for clinical trials. And then I started to write. I wrote as much as I could for the rest of the day and into the evening. When I couldn't take anymore, I headed out for dinner.
On my way home I started to get pings from several different directions. The "Sue"-club and some people in the "Dorland hospital" have contact with several medical advocates, and those advocates laid out a concept for how to speak the truth to the deny-ers. Unfortunately, what I had already written would need to be completely reworked. I was overly exhausted and mentally spent. I decided I'd have to try to get that work done in the morning, mere hours before I needed to appear before the deny-ers.
This morning I woke up, turned on my computer, and saw that my (Google) document had been completely modified! Admittedly, my initial reaction was panic. My sister completely changed my document and didn't make a copy! And then I started to read. She had somehow reconfigured this document into the exact style described by the advocates. It literally brought tears to my eyes to see how wonderfully written and clearly stated it had become. It was as if I went to bed, and a bunch of elves came out and did all of my work for me. I presented this newly minted argument to the deny-ers as written, and even delivered it along with peer reviewed papers and a copy of the California law requiring insurance companies to cover clinical trial costs. While I'm still hesitant to think that they will reverse their decision, as a team, we could not have covered it any better. I will know within the next week.
So my thanks go out to the "Sue"-club, my freighbor, and of course my fabulous family. Both of my sisters deserve tremendous praise for the document I used to fight the good fight. As I said to a friend of mine who commented on their brilliance, merge a lawyer with an experienced Drama/English Literature professor and that's what you get...and I couldn't have asked for anything more.
The rest of my time has primarily been spent trying to figure out how to pay for the trial. My "insurance" company, Kaiser Permanente, will not pay for the out-of-network surgery required by all of these trials. They would be happy to allow me into the trial if they could perform the surgery themselves. However, none of the trials can allow that due to FDA regulation. So here I sit in the middle of what clearly seems to me to be a financial clampdown of Kaiser. I submitted an appeal to their denial, and my appeal was...well...denied. I was offered, however, a personal 10 minute response to the deny-ers, live and in person. Today.
Now, according to them, I was denied coverage of this trial because "referral to the clinical trials [I] have requested is not medically indicated at this time because they lack efficacy in peer reviewed literature." And furthermore, "[My] treating neuro-oncologist...has offered to [me] treatment with a clinical trial with Tocagen or treatment with avastin/CCNU, which [I] have declined."
So, in 10 minutes I need to prove that (a) the trials I'm considering have strong evidence of efficacy (including peer reviewed literature), (b) the trials that are acceptable to Kaiser show far less efficacy than the vaccine trials, but require little financial contribution by Kaiser, thus indicating that their decisions are financial, not medical, and (c) the main thing that Kaiser is denying, the surgery required by the clinical trial, is, in and of itself, the most medically indicated treatment I could have given my current condition. Yes, that's a lot. My first step? Send out an e-mail to my family that says, "I need help!" Immediately they kicked into high gear, finding me several great peer reviewed articles and other information. I also touched base with the "Sue"-club, two friends who have a lot of experience dealing with Kaiser and with funding for clinical trials. And then I started to write. I wrote as much as I could for the rest of the day and into the evening. When I couldn't take anymore, I headed out for dinner.
On my way home I started to get pings from several different directions. The "Sue"-club and some people in the "Dorland hospital" have contact with several medical advocates, and those advocates laid out a concept for how to speak the truth to the deny-ers. Unfortunately, what I had already written would need to be completely reworked. I was overly exhausted and mentally spent. I decided I'd have to try to get that work done in the morning, mere hours before I needed to appear before the deny-ers.
This morning I woke up, turned on my computer, and saw that my (Google) document had been completely modified! Admittedly, my initial reaction was panic. My sister completely changed my document and didn't make a copy! And then I started to read. She had somehow reconfigured this document into the exact style described by the advocates. It literally brought tears to my eyes to see how wonderfully written and clearly stated it had become. It was as if I went to bed, and a bunch of elves came out and did all of my work for me. I presented this newly minted argument to the deny-ers as written, and even delivered it along with peer reviewed papers and a copy of the California law requiring insurance companies to cover clinical trial costs. While I'm still hesitant to think that they will reverse their decision, as a team, we could not have covered it any better. I will know within the next week.
So my thanks go out to the "Sue"-club, my freighbor, and of course my fabulous family. Both of my sisters deserve tremendous praise for the document I used to fight the good fight. As I said to a friend of mine who commented on their brilliance, merge a lawyer with an experienced Drama/English Literature professor and that's what you get...and I couldn't have asked for anything more.
Saturday, January 15, 2011
Quick update
I've heard from Dr. Yu at Cedars-Sinai, and it sounds like I'd fit in well with his vaccine clinical trial. I'm still waiting to hear from UCLA about their clinical trials, but the more I investigate and think about it, the more I'm starting to lean towards C-S. Even though I paid lots of money for the UCLA "2nd opinion", while C-S did it for free....
Next step, talk it over with my Kaiser neurooncologist Monday and hopefully nail down the final decision.
Next step, talk it over with my Kaiser neurooncologist Monday and hopefully nail down the final decision.
Wednesday, January 12, 2011
Hurry up...and wait
Over the past week, most of my time has been spent trying in so many ways to figure out what my final treatment plan will be. And I am a TERRIBLE planner. I've been gathering opinions from my oncologists and surgeons at Kaiser, UCSF, Cedars-Sinai, and now, hopefully UCLA. With each conversation I do feel like I'm one step closer to where I want to be, but I'm hoping that where I want to be isn't trying to slip away.
Here's the general layout of how things have gone. The initial discussions with my neurooncologist at Kaiser revolved around the remaining standard treatment, which would involve either surgery or radiosurgery, followed with Avastin and some other form of chemo. However, he did offer a 2nd opinion from the UCSF group to see if there are any interesting clinical trials that might serve a better purpose. One trial he suggested was called Toca-511, named after the company Tocagen. This trial is a Phase I trial with very little evidence in humans, but animal testing has shown marked improvements. The other trial that is buzzing in every glioblastomite's ear is the vaccine trial that UCSF is currently running. This trial requires a certain size tumor that is resectable so that enough vaccine can be developed from the extracted cells.
After manually carrying my medical records and images to UCSF, I was presented in front of the Tumor Board. From there I learned that (a) I would be a good candidate for the Tocagen trial, and (b) my tumor is likely too SMALL for the UCSF vaccine trial. I hate it when size really matters. It was also mentioned that the vaccine trial requires surgery at the trial site, and that in the past it has been difficult to get Kaiser to support any trials that require surgery. This was the beginning of what might by the largest concern overall. The most important opinion that I got, however, was that likely I should hold things like Avastin in my back pocket for times when I'll really need it, and instead should take advantage of clinical trials that show promise.
After that meeting, I began to research clinical trials further, and found another vaccine trial at UCLA and Cedars-Sinai. Their methods require resection of a much smaller tumor, giving me a stronger possibility of qualifying. I sent all of my medical records to those two teams along with a box of Poco Dulce chocolate (good idea Rat!)
In the meantime I had another meeting with Dr. Aghi at UCSF to talk about the Tocagen trial. He was very convincing about the possible efficacy of that trial, even though it's just started with very few results. In particular, he removed most of the major concerns regarding whether this trial will eliminate qualification for other trials in the future if needed. However, it sounded like this trial will essentially only attack the tumor that is currently active, whereas a vaccine trial can potentially attack all remaining cancer cells. One thing that was clear, UCLA was a partner on the Tocagen trial AND had a very interesting vaccine trial. I really need to talk to them to examine my best treatment options.
So where are we now? Well, UCLA has received all of my records and presented them in front of their Tumor Board. And? Drumroll please? They are mailing me the report to be received by the end of the week. Er?!? This is not the resolution I was hoping for. I did ask them directly if, while I wait for the mailman to show up, they could tell me if I might qualify for the vaccine trial. Still waiting for a reply on that one. Meanwhile, I'm hoping that should I get accepted to that trial, I will get the support I need from Kaiser, or this could be a pricey battle I'll be fighting down the line.
Here's the general layout of how things have gone. The initial discussions with my neurooncologist at Kaiser revolved around the remaining standard treatment, which would involve either surgery or radiosurgery, followed with Avastin and some other form of chemo. However, he did offer a 2nd opinion from the UCSF group to see if there are any interesting clinical trials that might serve a better purpose. One trial he suggested was called Toca-511, named after the company Tocagen. This trial is a Phase I trial with very little evidence in humans, but animal testing has shown marked improvements. The other trial that is buzzing in every glioblastomite's ear is the vaccine trial that UCSF is currently running. This trial requires a certain size tumor that is resectable so that enough vaccine can be developed from the extracted cells.
After manually carrying my medical records and images to UCSF, I was presented in front of the Tumor Board. From there I learned that (a) I would be a good candidate for the Tocagen trial, and (b) my tumor is likely too SMALL for the UCSF vaccine trial. I hate it when size really matters. It was also mentioned that the vaccine trial requires surgery at the trial site, and that in the past it has been difficult to get Kaiser to support any trials that require surgery. This was the beginning of what might by the largest concern overall. The most important opinion that I got, however, was that likely I should hold things like Avastin in my back pocket for times when I'll really need it, and instead should take advantage of clinical trials that show promise.
After that meeting, I began to research clinical trials further, and found another vaccine trial at UCLA and Cedars-Sinai. Their methods require resection of a much smaller tumor, giving me a stronger possibility of qualifying. I sent all of my medical records to those two teams along with a box of Poco Dulce chocolate (good idea Rat!)
In the meantime I had another meeting with Dr. Aghi at UCSF to talk about the Tocagen trial. He was very convincing about the possible efficacy of that trial, even though it's just started with very few results. In particular, he removed most of the major concerns regarding whether this trial will eliminate qualification for other trials in the future if needed. However, it sounded like this trial will essentially only attack the tumor that is currently active, whereas a vaccine trial can potentially attack all remaining cancer cells. One thing that was clear, UCLA was a partner on the Tocagen trial AND had a very interesting vaccine trial. I really need to talk to them to examine my best treatment options.
So where are we now? Well, UCLA has received all of my records and presented them in front of their Tumor Board. And? Drumroll please? They are mailing me the report to be received by the end of the week. Er?!? This is not the resolution I was hoping for. I did ask them directly if, while I wait for the mailman to show up, they could tell me if I might qualify for the vaccine trial. Still waiting for a reply on that one. Meanwhile, I'm hoping that should I get accepted to that trial, I will get the support I need from Kaiser, or this could be a pricey battle I'll be fighting down the line.
Friday, January 7, 2011
As the world turns....
The last few days have been spent trying to figure out what the best option for treatment might be. Most of it was spent on the internet, and I can't imagine how people managed to care for themselves before it existed! Sorry, I refuse to embarrass Gore by misquoting him, when in fact *I* invented the internet. Or at least - I work for the company that helped invent it....
But I digress. Today I had an appointment at UCSF talking with one of the fantastic oncologists there, Dr. Clarke. I was ably assisted by Gabrielle, a ridiculously amazing and caring "survivor" who has dedicated a lot of her time to battling brain cancer. Together we whittled down the options to a plan that seems to make sense - until you throw in my insurer. Kaiser. Up until now I have actually been very fond of them, and stuck with them even though I had an opportunity to change health plans at work. I'm really hoping not to regret that decision, but so far I've heard far too many comments on how the best clinical trials I can find, those with the most likely chance of long term survival, will likely not be supported by Kaiser. I am certainly not going to let that stop my choices, and we will see if they would really be so cold. I'm hoping they won't.
In terms of my list of choices, I am mostly looking at several trials involving vaccines created from the tumor itself. One trial is at UCSF, and two are down in Los Angeles (AE, I might be visiting you after all!) There is another Phase 1 trial involving retroviruses, paid for by the drug company supplying them (so Kaiser wouldn't deny that one). Unfortunately, since it is Phase 1, there isn't much evidence that it will work, and not enough evidence that it won't cause problems. I'll be talking with the head of that clinic at UCSF on Monday and maybe that information will persuade me one way or the other.
I really appreciate the kind words passed my way by everyone out there. It means a lot!
But I digress. Today I had an appointment at UCSF talking with one of the fantastic oncologists there, Dr. Clarke. I was ably assisted by Gabrielle, a ridiculously amazing and caring "survivor" who has dedicated a lot of her time to battling brain cancer. Together we whittled down the options to a plan that seems to make sense - until you throw in my insurer. Kaiser. Up until now I have actually been very fond of them, and stuck with them even though I had an opportunity to change health plans at work. I'm really hoping not to regret that decision, but so far I've heard far too many comments on how the best clinical trials I can find, those with the most likely chance of long term survival, will likely not be supported by Kaiser. I am certainly not going to let that stop my choices, and we will see if they would really be so cold. I'm hoping they won't.
In terms of my list of choices, I am mostly looking at several trials involving vaccines created from the tumor itself. One trial is at UCSF, and two are down in Los Angeles (AE, I might be visiting you after all!) There is another Phase 1 trial involving retroviruses, paid for by the drug company supplying them (so Kaiser wouldn't deny that one). Unfortunately, since it is Phase 1, there isn't much evidence that it will work, and not enough evidence that it won't cause problems. I'll be talking with the head of that clinic at UCSF on Monday and maybe that information will persuade me one way or the other.
I really appreciate the kind words passed my way by everyone out there. It means a lot!
Subscribe to:
Comments (Atom)